Article featured on Modern Orthopedics
You’re lifting the canoe onto your car’s roof rack when you feel it again—that pain and weakness through your shoulder and down your arm. Rubbing your shoulder joint, you wonder what on earth is going on and how you’re going to address it.
If you’re experiencing unexplained pain in your shoulder, neck, arms, or upper back, shoulder bone spurs could be one of the possible culprits. While relatively common, these bony protrusions can significantly impact your daily routine and quality of life.
Fortunately, shoulder bone spurs are treatable in a variety of different ways, depending on their severity and your lifestyle goals. Below, we’ll explore what they are, how they’re diagnosed, and provide an overview of common treatment options.
If you suspect that you may have shoulder bone spurs, making an appointment with your orthopedic surgeon as soon as possible will help you determine the best course of action.
What Are Shoulder Bone Spurs?
Bone spurs (known medically as osteophytes) are bony projections that develop along the edges of bones. Often, they’re small, smooth, and go unnoticed in the body without causing any symptoms. But when bone spurs press or rub against other bones or soft tissues (including ligaments, tendons, and nerves), the results can be painful and seriously impede your day-to-day routine.
Why do bone spurs form? Most often, they develop in response to injury or inflammation in order to protect a joint or area of the body that has been damaged. Unfortunately, they sometimes also cause more damage in the process.
While bone spurs can form in many different parts of the body, including the hips, knees, and spine, the shoulder is one of the most common areas where they often become problematic. When bone spurs form under the acromion (the tip of the outer edge of your shoulder blade or scapula), they can cause significant discomfort and require proactive treatment.
Symptoms of Shoulder Bone Spurs
Because the size, location, and impact of shoulder bone spurs on the body vary from person to person, they can present in a variety of ways. Depending on the circumstances, symptoms of shoulder bone spurs may include one or more of the following:
- Shoulder pain
- Neck pain
- Pain in the upper back or arms
- Tingling or numbness
- Tenderness
- Weakness
- Visible inflammation
- Stiffness
- Muscle spasms
- Decreased range of motion
- A visible lump under the skin (large bone spurs only)
- Tearing of tendons or ligaments (in severe cases)
Causes of Shoulder Bone Spurs
Bone spurs form in response to joint inflammation. But inflammation always has an underlying cause. Underlying causes of bone spurs often include:
- Arthritis (rheumatoid arthritis, osteoarthritis, or degenerative arthritis)—Bone spurs form in response to the breakdown of cartilage at the ends of bones in an attempt to repair the damage.
- Acute injury—Acute shoulder injuries can be caused by direct impact or other damaging incidents.
- Repetitive Injury—People who regularly perform repetitive overhead movements are at risk for the development of shoulder bone spurs along with injury to the rotator cuff tendons.
- Genetics—Patients with a family history of bone spurs (or osteochondromas) may experience shoulder bone spurs more frequently than the general population.
Diagnosis of Shoulder Bone Spurs
Because the symptoms of shoulder bone spurs are varied and often exist within the context of a broader condition or injury, the most conclusive way to diagnose their presence is via a visual confirmation. Bone spurs are often diagnosed by X-ray, MRI, CT scan, or ultrasound. Your orthopedic surgeon will recommend the diagnostic method they believe will be most appropriate for your symptoms and circumstances.
Treatment for Shoulder Bone Spurs
If you’re diagnosed with shoulder bone spurs, your individual treatment plan will take into account your current level of pain, lifestyle, and personal goals. Reducing pain and avoiding future injuries will always be the priority. Your orthopedic surgeon will outline and consider less invasive treatment options before recommending surgery. Ultimately, your preferred course of treatment will be up to you.
Non-Surgical Treatments
In cases with mild symptoms, the following non-surgical treatments may be ideal:
Physical Therapy
A physical therapist can provide an exercise program tailored to your needs in combination with treatments such as deep tissue massage, ultrasound and more. Physical therapy can often drastically reduce the pain associated with shoulder bone spurs. Decreasing the health of the surrounding tissues with stretching and strengthening, can decrease inflammation and therefore pain associated with bone spurs.
Medication
The most common medications associated with the treatment of shoulder bone spurs are over-the-counter anti-inflammatory drugs and pain relievers.
Rest and Lifestyle Modifications
Rest can sometimes work wonders for bone spur pain. Avoiding triggering movements and overuse in your daily life can promote effective healing—even the reabsorption of bone spurs by the body.
Minimally Invasive Procedures
If your body isn’t responding to the simple, non-surgical treatment options listed above, it may be time to consider a minimally invasive procedure.
Corticosteroid Injections
Therapeutic steroid injections can sometimes reduce pain and increase your range of motion.
Arthroscopic Surgery
Arthroscopic surgery for bone spurs in the shoulder joint involves trimming or removing bone spurs to open up space and relieve pressure on bones, ligaments, and tissues.
Surgical Treatments
Open Surgery
Open surgery is typically the last resort and is only considered in severe cases where bone spurs are seriously impacting your quality of life. Surgeries such as subacromial decompression (which can involve removing spurs and thickened ligaments as well as resurfacing shoulder bones) and shoulder arthroplasty (which is a replacement of the shoulder joint) often have excellent outcomes but are major procedures that involve a significant investment of time and require extensive rehabilitation.
Conclusion
To conclude, shoulder bone spurs are a common cause of shoulder pain and discomfort that can range from mild to severe. They typically occur as the result of an underlying cause or condition and require thoughtful and knowledgeable treatment.
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, foot and ankle conditions, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic and podiatric surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
17355 Lower Boones Ferry Rd Suite 100A
Lake Oswego, OR 97035
Hours
Monday–Friday
8:00am – 4:30pm

Scoliosis: Causes and Treatments
in Back PainArticle featured on Johns Hopkins Medicine
What is scoliosis?
The spine is made up of a stack of rectangular-shaped building blocks called vertebrae. When viewed from behind, the spine normally appears straight. However, a spine affected by scoliosis is curved — often appearing like an S or C — with a rotation of the vertebrae. This curvature gives the appearance that the person is leaning to one side.
Scoliosis is determined when the curvature of the spine measures 10 degrees or greater on an X-ray. Spinal curvature from scoliosis may occur on the right or left side of the spine, or on both sides in different sections. Both the thoracic (mid) and lumbar (lower) spine may be affected by scoliosis. Scoliosis is a type of spinal deformity.
In more than 80 percent of cases, the cause of scoliosis is unknown — a condition called idiopathic scoliosis. In other cases, scoliosis may develop as a result of degeneration of the spinal discs, as seen with arthritis, osteoporosis or as a hereditary condition that tends to run in families.
What are the different types of scoliosis?
Congenital Scoliosis
In congenital scoliosis, spinal curvature develops because of misshapen vertebrae. The diagnosis of congenital scoliosis may be made in early infancy if outward signs are present, but many cases are diagnosed later in childhood.
As a child grows, scoliosis may worsen, and asymmetries in the body may develop. Typically, congenital scoliosis is treated with a “watch and wait” approach. Surgery is considered only if a curve is clearly getting worse and the child is facing ongoing deformity and risk of future pain.
Idiopathic Scoliosis
Doctors, nurses and scientists have been studying the natural history and genetics of scoliosis for decades, but to this day, the cause of idiopathic scoliosis is still unknown. But we do know that the most common time for idiopathic scoliosis to develop is at the onset of adolescence, or around the age of 10. We also know that growth can make it worse, and we should be most concerned about scoliosis in a child that has significant growth remaining.
When diagnosed in children 2 or younger, this type of scoliosis is called infantile idiopathic scoliosis.
Neuromuscular Scoliosis
A child with an underlying neuromuscular condition is at higher risk for developing scoliosis. A straight spine requires normal muscle balance and strength in the torso. In conditions such as cerebral palsy, spina bifida and muscular dystrophy, the muscles are often weak and unbalanced, leading to the development of a spinal curvature.
A child with neuromuscular scoliosis is given the option of wearing a scoliosis brace that may slow or prevent the worsening of the condition. Surgical intervention is offered when the curve has reached the tipping point of 50 degrees. Over time, these curves will continue to worsen, leading to progressive imbalance of the torso. Beyond 80 degrees, breathing challenges develop as space for the lungs decreases.
What are the symptoms of scoliosis?
The following are the most common symptoms of scoliosis. However, each individual may experience symptoms differently. Symptoms may include:
The symptoms of scoliosis may resemble other spinal conditions or deformities, or may be a result of an injury or infection. Always consult your doctor for a diagnosis.
Symptoms that are not commonly associated with idiopathic scoliosis are back pain, leg pain, and changes in bowel and bladder habits. If a person is experiencing these types of symptoms, he or she requires immediate further medical evaluation by a doctor to determine the cause of the symptoms.
How is scoliosis diagnosed?
Early detection of scoliosis is most important for successful treatment. In addition to a complete medical history and physical examination, an X-ray is the primary diagnostic tool for scoliosis. In establishing a diagnosis of scoliosis, the doctor measures the degree of spinal curvature on the X-ray.
The following additional diagnostic procedures may be performed for nonidiopathic curvatures, atypical curve patterns or congenital scoliosis:
How is scoliosis treated?
The goal of treatment is to stop the progression of the curve and prevent deformity. Observation and repeated examinations — also referred to as the “watch and wait” approach — may be necessary to determine if the spine is continuing to curve. These are used when a person has a curve that is less than 20 degrees and who is still growing.
For actively growing children with scoliosis curves between 20 and 50 degrees, bracing is recommended. An external torso brace, or TLSO, is worn for a prescribed number of hours. The brace applies corrective pressure to the growing spine, preventing further worsening of the scoliosis. Surgery is a recommended treatment option for a child with severe scoliosis or a curve that has worsened to more than 50 degrees.
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, foot and ankle conditions, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic and podiatric surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
17355 Lower Boones Ferry Rd Suite 100A
Lake Oswego, OR 97035
Hours
Monday–Friday
8:00am – 4:30pm
Common Reason for Foot Pain and Problems
in Foot PainArticle featured on Brigham and Women’s Hospital
Anatomy of the foot
The foot is one of the most complex parts of the body. It’s made up of 26 bones connected by many joints, muscles, tendons, and ligaments. The foot is at risk of many stresses. Foot problems can cause pain, inflammation, or injury. These problems can result in limited movement and mobility.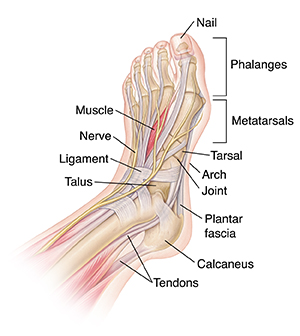
What are the different types of foot problems?
Foot pain is often caused by incorrect foot function. Shoes that don’t fit well can make foot problems worse and, in some cases, cause them. Shoes that fit correctly and give good support can prevent irritation to the foot joints and skin. There are many types of foot problems that affect the heels, toes, nerves, tendons, ligaments, and joints of the foot.
The symptoms of foot problems may look like other health conditions and problems. Always see your healthcare provider for a diagnosis.
What are heel spurs?
A heel spur is a bone growth on the heel bone. It’s often located on the underside of the heel bone where it attaches to the plantar fascia. This is a long band of connective tissue running from the heel to the ball of the foot. This connective tissue holds the arch together and acts as a shock absorber during activity. The plantar fascia can be overstretched from running, wearing poor-fitting shoes, or being overweight. Then pain can result from the stress and inflammation of the tissue pulling on the bone. Over time, the body builds extra bone in response to this stress, causing heel spurs. Treatment methods may include:
What is a corn?
Corns are yellowish, callus growths that occur on top of the toes. Corns develop because of irritation or stress. Often, a corn develops where a toe rubs against a shoe or another toe. Corns can cause extreme discomfort and pain. Treatment may include:
To prevent corns, always buy shoes that fit correctly.
What is a bunion?
A bunion is a bulge of bone or tissue around the joint of the great toe or small toe. Bunions may occur at the base of the great toe or at the base of the little toe. They often occur when the joint is stressed over a period of time. Women get bunions more often than men do because they may wear tight, pointed, and confining shoes. Bunions can also be a result of arthritis, which often affects the big toe joint.
Treatment of bunions may vary depending on the pain and deformity. Treatment may include:
What is Morton neuroma?
Morton neuroma is a buildup of noncancer (benign) tissue in the nerves running between the long bones of the foot. Morton neuroma occurs when 2 bones rub together and squeeze the nerve between them. Most often, neuromas develop between the bones leading to the third and fourth toes. Morton neuroma often causes swelling, tenderness, and pain. If the pain becomes severe, it may cause tingling, numbness, and burning in the toes. It often occurs after standing or walking for a long period of time. Treatment for this condition may involve rest or a change in footwear that doesn’t restrict the foot. If the problem persists, cortisone injections or surgery may be considered.
What are hammertoes?
A hammertoe is when the toe bends or curls downward. This causes the middle joint of the affected toe to poke out. Tight-fitting shoes that put pressure on the hammertoe often make this condition worse. Often a corn develops at this site. Treatment for hammertoes may include:
What is an ankle sprain?
An ankle sprain is an injury to the ligaments in the ankle. Ligaments are tough bands of elastic tissue that connect bones to each other. Ankle sprains may occur if the ankle rolls, turns, or twists beyond its normal range of motion. Ankle sprains may be caused by awkward foot placement, irregular surfaces, weak muscles, loose ligaments, or wearing shoes with spiked heels.
The symptoms of a sprain will depend on how severely the ligaments are stretched or torn, but usually include swelling, pain, or bruising. Treatment will depend on the severity of the sprain, but may include:
What is a foot fracture?
With 26 bones in a single foot, almost any of them can be broken. Many breaks or fractures don’t need surgery, or even a cast. They will heal on their own with some support. When a foot is fractured, the site of the fracture usually is painful and swollen. The site of the fracture will determine the course of treatment, if needed, including:
What is foot pain?
Foot pain can get in the way of an active lifestyle. Foot pain can have many sources, from fractures and sprains to nerve damage. Listed below are 3 common areas of pain in the foot and their causes:
Plantar fasciitis is more common in women, people who are overweight, people with jobs that need a lot of walking or standing on hard surfaces, people with flat feet, and people with high arches. Walking or running, especially with tight calf muscles, may also cause the condition.
Treatment may include:
Achilles tendonitis is caused by overuse of the tendon and calf muscles. Symptoms may include mild pain after exercise that gets worse gradually, stiffness that improves after the tendon warms up, and swelling. Treatment may include:
Diabetes and vascular disease
Diabetes affects the nerves, blood vessels, and blood flow throughout the whole body, including the legs and feet. People with diabetes need to check their feet regularly to identify sores or wounds on their feet before complications develop. And to help manage diabetes-related foot problems, they may need to see a healthcare provider and orthopedic specialist, and sometimes a vascular specialist.
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, foot and ankle conditions, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic and podiatric surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
17355 Lower Boones Ferry Rd Suite 100A
Lake Oswego, OR 97035
Hours
Monday–Friday
8:00am – 4:30pm
What You Need to Know About Navigating Shoulder Instability
in Shoulder InjuriesArticle featured on OrthoUnited
What Is Shoulder Instability?
Shoulder instability occurs when the shoulder joint is too loose and frequently slips out of place. The shoulder is a ball-and-socket joint, where the ball (the head of the humerus) fits into the shoulder blade’s socket (the glenoid).
When the ligaments, tendons, and muscles surrounding the shoulder joint are stretched or torn, they can no longer keep the joint in place. This condition can lead to partial or complete dislocations and a sensation of the shoulder “giving out.”
People suffering from shoulder instability often experience pain, weakness, and a limited range of motion. The condition can be a result of trauma, repetitive use, or a structural abnormality of the shoulder.
How Does It Develop?
Shoulder instability can occur in several ways:
How Is It Diagnosed?
Diagnosing shoulder instability begins with a comprehensive medical history and physical examination. Your healthcare provider will ask about your symptoms, previous injuries, and activity level. During the physical examination, the doctor will check for signs of instability, such as abnormal shoulder joint movement or a popping sensation when the shoulder is moved.
Imaging tests like X-rays, MRI, or CT scans may provide a more detailed view of the shoulder joint. These tests help identify any structural damage to the bones, ligaments, or cartilage that may contribute to the instability.
A proper diagnosis is crucial because the treatment plan will vary depending on the severity and type of shoulder instability. If you suspect you have shoulder instability, consult a specialist immediately for an accurate diagnosis.
Treatment Options for Shoulder Instability
Treatment for shoulder instability depends on the extent of the condition and the patient’s lifestyle. Here are some of the standard treatment options:
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, foot and ankle conditions, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic and podiatric surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
17355 Lower Boones Ferry Rd Suite 100A
Lake Oswego, OR 97035
Hours
Monday–Friday
8:00am – 4:30pm
Prevent Injuries with Shoulder Stretches & Hamstring Stretches
in Legs & Feet, Shoulder InjuriesArticle featured on NY Orthopedics
Why are Shoulder and Hamstring Stretches Important?
Stretching plays a critical role in maintaining flexibility, improving range of motion, and reducing muscle tension. Loose and flexible muscles are less likely to experience strains or tears during physical activities like backyard sports.
Regular stretching helps to improve blood flow to the muscles, enhancing their ability to recover quickly and efficiently after exertion. Stretching is especially important for those over the age of 30, those with chronic injuries, or those prone to muscular tears. Sudden bursts of activity, like those in football or baseball, can put extra stress on the muscles and joints, making stretching beforehand that much more necessary.
Shoulder Stretches for Injury Prevention
Shoulder injuries are among the most common in many sports, particularly those that involve throwing or overhead movements like beach volleyball. To prevent these injuries, it’s important to keep your shoulder muscles and joints flexible and strong with some targeted stretches. Here are some common, easy-to-do stretches that can help you limber up before serving up some heat:
Hamstring Stretches for Flexibility
Hamstring injuries are another common issue, especially in sports that involve running and jumping. Keeping your hamstrings flexible with targeted stretches can prevent strains and improve your overall performance. Here are some hamstring stretches to help you stay loose for those one-on-ones:
Incorporating Stretches into Your Routine
To maximize the benefits of stretching, you should not only stretch before physical activity but incorporate stretching into your daily routine. Remember that stretches are meant to build muscle, joint flexibility, and strength. This doesn’t happen after one stretching session. Like any other exercise, it takes time and discipline to reap the full rewards.
Fortunately, most people notice results relatively quickly. You can start small with a gentle warm-up as you get out of bed to get your blood flowing before moving into the stretches—something light like jumping jacks. Then, try out some of the stretches we’ve provided here or integrate more full-body stretches.
By properly stretching your shoulders and hamstrings, you can significantly reduce the risk of injuries!
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, foot and ankle conditions, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic and podiatric surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
17355 Lower Boones Ferry Rd Suite 100A
Lake Oswego, OR 97035
Hours
Monday–Friday
8:00am – 4:30pm
Are Standing Desks Good for Your Back?
in Ergonomics, Wellness Tips, Working From Home- TipsArticle featured on Summit Orthopedics
Standing desks promise many benefits, including better overall health and less back pain. Research is ongoing into what, if any, benefits a standing desk might actually have, but if you’re used to sitting for long hours and staring at a computer each day, you know how tough all that sitting can be on your back and neck. Can a standing desk help?
The connections between sitting and back pain
One reason sitting for long periods of time can cause backaches is that it puts more pressure on the discs that cushion the spine’s bony vertebrae. Sitting for a long time can also cause muscles in the back to get stiff, creating soreness. If you’re sitting with poor posture, that can make the effects worse. Slouching can put more stress on the spinal ligaments and result in increased pressure on some parts of the spine. Standing desks seek to solve these problems.
Why might it be better to stand at a standing desk?
If your work requires you to be on a computer for most or all of your workday, a standing desk gives you a way to do that work while standing. Here are some potential benefits of standing more during the day:
Note Some people — those with vascular problems or who are at increased risk of swelling in their lower limbs — might have increased health risks from a standing desk. Talk with your healthcare provider before choosing to try a standing desk.
How can I get started with a standing desk?
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, foot and ankle conditions, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic and podiatric surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
17355 Lower Boones Ferry Rd Suite 100A
Lake Oswego, OR 97035
Hours
Monday–Friday
8:00am – 4:30pm
Common Fall Sports Injuries (And How to Prevent Them)
in Sports Medicine, Sports Related InjuriesArticle featured on Towson Orthopaedic Associates
When the crisp autumn air cuts through the dog days of summer, runners are on their mark. The fall season starts many high-intensity sports for teens and adults, which means injuries can increase when coming off of a break. Practicing good habits like stretching can prevent injuries so you can get ready, get set, and go with your favorite sport this fall.
Fall Season Sports
Many fall sports have running at their core. Football, soccer, and cross country running come to mind. But sports like tennis, lacrosse, and volleyball also require strong, repetitive motion. Strength and cardiovascular training are essential to success and safety in any sport.
Typical Sports from September to November:
Common Fall Sports Injuries
All types of sports and athletic activities come with an increased risk of injury. Typical injuries include leg injuries, knee injuries, arm injuries, shoulder injuries, and head injuries. The most common injuries are:
A Concussion is a brain injury that can occur in any sport, but is more common in contact sports—such as football or field hockey—and in sports like soccer where the head is used in play. Any blows to the head should be taken seriously to prevent a more serious head injury. Learn to recognize the following signs of concussion:
Playing through a concussion can lead to more serious injury and prolonged symptoms which can negatively impact mental state and abilities.
Fractures are bone breaks that require immediate medical attention. There are many different types of fractures. These include:
Strains occur from a sudden awkward movement or overuse of a muscle in the upper and lower body. Muscle strain can affect both novice and experienced athletes. Exerting a strained muscle can worsen the injury. Recognize these symptoms of a strain to take a time out:
Sprains are partial or complete tears of a ligament within a joint and most commonly occur in the ankle, wrist, or knee. Most are minor injuries, however, an anterior cruciate ligament—or ACL tear—is a common injury that affects the ligament that stabilizes the knee. It is a severe injury that requires rehabilitation and/or surgery. Signs of a sprain include:
Strains and sprains are similar injuries that are treated with PRICE, an acronym for the treatment protocol of: Protection, Rest, Ice, Compression, and Elevation. Minor sprains should respond to PRICE and an anti-inflammatory painkiller.
Shin Splints are overuse injuries that commonly afflict runners. It is an injury of the soft tissue that holds the muscle to the bone and is caused by a rapid increase in intensity or frequency of running, improper shoes, or occasional flat feet.. Shin splints can occur with any sport that involves strenuous running, like soccer or field hockey. To prevent shin splints, stretch before any physical activity and make sure to get plenty of rest between active sessions. Replace your shoes at regular intervals—for runner’s, that is every 300-500 miles.
Patellofemoral syndrome, commonly known as runner’s knee, is a knee injury that causes pain when the cartilage in the kneecap becomes irritated. Repetitive squatting or crouching motions, like those used in volleyball. Treatment for runner’s knee typically includes the PRICE method, kinesiology taping or bracing, and physical therapy focused on strengthening the core, knee, and surrounding muscle groups.
Preventing Sports Injuries
Being aware of what kinds of injuries to expect in the fall sports season makes sports injury prevention easier.
This simple checklist can help to prevent injury in any sport:
Following these injury prevention tips can prepare the body for strenuous activity and keep you off the bench this season. Remember, getting back into the swing of things this autumn doesn’t have to be a drag.
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, foot and ankle conditions, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic and podiatric surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
17355 Lower Boones Ferry Rd Suite 100A
Lake Oswego, OR 97035
Hours
Monday–Friday
8:00am – 4:30pm
Posture Perfect: Improving Alignment for Back Health
in Back PainArticle featured on Orthopaedic Associates
In our busy lives, we often forget the significance of good posture. Did you know that maintaining proper alignment can have a profound impact on your spinal health and overall quality of life?
In this article, we will explore the importance of posture and how you can work toward having better posture for a healthier you.
The Importance of Good Posture
Good posture does more than just keep you looking confident. It ensures that your body functions optimally by:
When it comes to back health, posture plays a pivotal role. A well-aligned spine reduces stress on muscles and ligaments, decreasing the risk of chronic pain and degenerative diseases.
Steps to Improve Posture
Improving your posture is a proactive approach to maintaining a healthy back and overall well-being. Here are steps you can take to enhance your posture:
1. Awareness and Identification
The first step to better posture is self-awareness. Pay attention to how you sit, stand, and move throughout the day and identify any habits that contribute to poor posture. This may include:
2. Regular Posture Checks
Set reminders to check your posture regularly, especially if you have a desk job or spend hours on a computer. Ensure that:
Making these adjustments a habit can significantly improve your posture over time.
3. Core Strengthening
Maintaining a strong core is an essential component of good posture. Incorporate core-strengthening exercises into your fitness routine. Planks, bridges, and leg raises are all effective exercises that target the muscles supporting your spine.
4. Stretching Exercises
Stretching helps alleviate muscle tension and promotes flexibility. Focus on stretching your:
These stretches can counteract the effects of prolonged sitting and contribute to better posture.
5. Proper Ergonomics
If you have a desk job, make sure that your workspace is ergonomic. Level your chair, desk, and laptop or computer monitor to promote good posture. You should ensure that your chair supports your lower back and that your screen is at eye level to reduce strain on your neck.
6. Posture-Friendly Furniture
Invest in furniture that encourages good posture. Supportive chairs with lumbar support, ergonomic pillows, and standing desks can all contribute to maintaining proper alignment.
7. Mindful Sitting and Standing
Be mindful of your posture while you are sitting or standing. Imagine a string pulling the top of your head toward the ceiling to help you sit or stand tall. You should also distribute your body weight evenly between both feet when standing to prevent favoring one side.
8. Use Props
Consider using props, like cushions or lumbar rolls, to maintain correct spinal alignment while sitting. These props can help you maintain the natural curve of your lower back.
9. Regular Breaks
Don’t forget to pause and rest frequently throughout the day, particularly when your work involves minimal movement. Take a moment to stand up, stretch out your muscles, and walk around every hour. This can ward off tight muscles and encourage healthier posture.
10. Consult a Professional
If you are struggling with posture issues or experiencing persistent back pain, consult a healthcare provider or physical therapist. They can provide personalized guidance, exercises, and therapies to address your specific posture-related concerns.
By incorporating these steps into your daily routine and being mindful of your posture, you can make significant progress toward achieving better alignment and a healthier back.
When to Seek Medical Attention for Back Pain
While self-care can help with back pain, certain signs warrant a visit to a healthcare provider. Common signs you should seek medical attention for your back pain include:
In these cases, seeking medical advice is essential for a thorough evaluation and appropriate treatment.
Remember, early detection and intervention can lead to better outcomes for back pain and related conditions.
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, foot and ankle conditions, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic and podiatric surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
17355 Lower Boones Ferry Rd Suite 100A
Lake Oswego, OR 97035
Hours
Monday–Friday
8:00am – 4:30pm
Arthritis of the Neck
in Arthritis, Neck Injuries, Neck PainArticle featured on TriHealth
Arthritis of the Neck
Natural wear and tear of the cervical spine causing arthritis of the neck. As you age, the discs that serve as cushions between vertebrae begin to bulge, shrink or weaken. This allows the vertebrae to start collapsing on one another. This causes pain, stiffness and loss of range of motion. Your body responds to these changes by growing new bone (bone spurs), which can narrow the area around the spine.
Arthritis of the neck causes
Arthritis of the neck (cervical spondylosis) is most often a result of aging. It can also be caused by:
Arthritis of the neck symptoms
Many people with arthritis of the neck (cervical spondylosis) don’t experience any symptoms. However, some symptoms may include:
Arthritis of the neck treatment
Your treatment will depend on the cause of the pinched nerve. Treatment may include:
Generally, surgery is not needed to treat arthritis. Your provider may recommend surgery if your arthritis is causing another cervical spine condition, like a pinched nerve.
Arthritis of the neck risk factors
You may be at higher risk of developing arthritis in the neck if you:
Arthritis of the neck prevention
Nearly everyone over age 60 will develop cervical spondylosis. But, you can take steps to reduce your risk and minimize your pain:
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, foot and ankle conditions, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic and podiatric surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
17355 Lower Boones Ferry Rd Suite 100A
Lake Oswego, OR 97035
Hours
Monday–Friday
8:00am – 4:30pm
3 Ways To Treat Shoulder Bone Spurs
in Bone HealthArticle featured on Modern Orthopedics
You’re lifting the canoe onto your car’s roof rack when you feel it again—that pain and weakness through your shoulder and down your arm. Rubbing your shoulder joint, you wonder what on earth is going on and how you’re going to address it.
If you’re experiencing unexplained pain in your shoulder, neck, arms, or upper back, shoulder bone spurs could be one of the possible culprits. While relatively common, these bony protrusions can significantly impact your daily routine and quality of life.
Fortunately, shoulder bone spurs are treatable in a variety of different ways, depending on their severity and your lifestyle goals. Below, we’ll explore what they are, how they’re diagnosed, and provide an overview of common treatment options.
If you suspect that you may have shoulder bone spurs, making an appointment with your orthopedic surgeon as soon as possible will help you determine the best course of action.
What Are Shoulder Bone Spurs?
Bone spurs (known medically as osteophytes) are bony projections that develop along the edges of bones. Often, they’re small, smooth, and go unnoticed in the body without causing any symptoms. But when bone spurs press or rub against other bones or soft tissues (including ligaments, tendons, and nerves), the results can be painful and seriously impede your day-to-day routine.
Why do bone spurs form? Most often, they develop in response to injury or inflammation in order to protect a joint or area of the body that has been damaged. Unfortunately, they sometimes also cause more damage in the process.
While bone spurs can form in many different parts of the body, including the hips, knees, and spine, the shoulder is one of the most common areas where they often become problematic. When bone spurs form under the acromion (the tip of the outer edge of your shoulder blade or scapula), they can cause significant discomfort and require proactive treatment.
Symptoms of Shoulder Bone Spurs
Because the size, location, and impact of shoulder bone spurs on the body vary from person to person, they can present in a variety of ways. Depending on the circumstances, symptoms of shoulder bone spurs may include one or more of the following:
Causes of Shoulder Bone Spurs
Bone spurs form in response to joint inflammation. But inflammation always has an underlying cause. Underlying causes of bone spurs often include:
Diagnosis of Shoulder Bone Spurs
Because the symptoms of shoulder bone spurs are varied and often exist within the context of a broader condition or injury, the most conclusive way to diagnose their presence is via a visual confirmation. Bone spurs are often diagnosed by X-ray, MRI, CT scan, or ultrasound. Your orthopedic surgeon will recommend the diagnostic method they believe will be most appropriate for your symptoms and circumstances.
Treatment for Shoulder Bone Spurs
If you’re diagnosed with shoulder bone spurs, your individual treatment plan will take into account your current level of pain, lifestyle, and personal goals. Reducing pain and avoiding future injuries will always be the priority. Your orthopedic surgeon will outline and consider less invasive treatment options before recommending surgery. Ultimately, your preferred course of treatment will be up to you.
Non-Surgical Treatments
In cases with mild symptoms, the following non-surgical treatments may be ideal:
Physical Therapy
A physical therapist can provide an exercise program tailored to your needs in combination with treatments such as deep tissue massage, ultrasound and more. Physical therapy can often drastically reduce the pain associated with shoulder bone spurs. Decreasing the health of the surrounding tissues with stretching and strengthening, can decrease inflammation and therefore pain associated with bone spurs.
Medication
The most common medications associated with the treatment of shoulder bone spurs are over-the-counter anti-inflammatory drugs and pain relievers.
Rest and Lifestyle Modifications
Rest can sometimes work wonders for bone spur pain. Avoiding triggering movements and overuse in your daily life can promote effective healing—even the reabsorption of bone spurs by the body.
Minimally Invasive Procedures
If your body isn’t responding to the simple, non-surgical treatment options listed above, it may be time to consider a minimally invasive procedure.
Corticosteroid Injections
Therapeutic steroid injections can sometimes reduce pain and increase your range of motion.
Arthroscopic Surgery
Arthroscopic surgery for bone spurs in the shoulder joint involves trimming or removing bone spurs to open up space and relieve pressure on bones, ligaments, and tissues.
Surgical Treatments
Open Surgery
Open surgery is typically the last resort and is only considered in severe cases where bone spurs are seriously impacting your quality of life. Surgeries such as subacromial decompression (which can involve removing spurs and thickened ligaments as well as resurfacing shoulder bones) and shoulder arthroplasty (which is a replacement of the shoulder joint) often have excellent outcomes but are major procedures that involve a significant investment of time and require extensive rehabilitation.
Conclusion
To conclude, shoulder bone spurs are a common cause of shoulder pain and discomfort that can range from mild to severe. They typically occur as the result of an underlying cause or condition and require thoughtful and knowledgeable treatment.
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, foot and ankle conditions, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic and podiatric surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
17355 Lower Boones Ferry Rd Suite 100A
Lake Oswego, OR 97035
Hours
Monday–Friday
8:00am – 4:30pm
The Lowdown on How Running Affects Your Knees
in Knee Injuries, Knee Pain, Legs & Feet, Sports Related InjuriesArticle featured on Healthline
Lacing up and hitting the pavement for a run is great exercise. It can also be therapeutic, lower your stress levels, and boost your sleep quality, among other benefits.
But given running’s repetitive impact, it can be hard on your body, too. Many wonder whether running harms their knees, specifically.
This article investigates that question, finds the answer, and shares how to take care of your knees when you run.
Is running bad for your knees?
Running is not bad for your knees; running with poor form is bad for your knees.
In fact, most knee injuries caused by running are overuse injuries, meaning you’re putting more stress on your body than it can handle.
Whether that’s ramping up your training schedule too quickly or not resting enough between runs, running too many miles before your muscles, bones, joints, and cartilage are ready for more can increase your risk of injury.
What the science says
Quite a bit of research has investigated running’s effects on the knees .
One study followed a group of long-distance runners, as well as a nonrunner control group, for 18 years. Through a series of X-rays over the nearly two decades, researchers monitored for any presence of osteoarthritis in the knees.
The study results showed that running among healthy older adults was not associated with more prevalent osteoarthritis. In fact, at the end of the study, 20% of the runners showed signs of osteoarthritis, compared with 32% of the nonrunners.
Another study suggests that running may be beneficial for the knees.
Researchers used gait analysis and computer modeling to confirm that running does place a higher load on the knees than walking. Yet, it also causes the bone and cartilage of the knee to adapt, potentially leading to stronger knees overall.
And what if you already have knee pain? Is running completely off the table for you? Research says not necessarily.
A recent study including 82 middle-age volunteers looked at the short-term effects of long-distance running on knee joints using magnetic resonance imaging (MRI).
Pre-training MRIs showed signs of asymptomatic damage to several knee structures in the majority of the participants. After the marathon, the MRIs showed a reduction in tibia and femoral bone damage. However, the MRIs also showed patellar cartilage deterioration.
What does all of this mean? Don’t forgo running because you’re afraid it may cause knee pain. But, as with every activity, listen to your body. When pain occurs, investigate why it might be happening.
Variables that can make running harder on your knees
However, there are a few variables that can make running hard on your knees. These include:
Warning signs your knees may need attention
If you develop any pain around the knee — including above, below, or behind the kneecap — during a run, your body is trying to tell you something. Regardless of whether the pain is dull or sharp, the best course of action is to stop running and rest.
Some common knee injuries in runners include:
If knee pain stops you from running, apply ice to the area and take it easy. If after a few days’ rest your knee is still bothering you, see your doctor for further evaluation.
Tips for protecting your knees when you run
Beyond running with proper form and wearing the right shoes, there are a few other things you can do to protect your knees while you run:
The bottom line
Don’t let a fear of hurting your knees stop you from running. By taking the appropriate precautions — strength training, stretching, wearing proper gear, and being conservative in your training — the benefits of running may very well outweigh the risks.
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, foot and ankle conditions, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic and podiatric surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
17355 Lower Boones Ferry Rd Suite 100A
Lake Oswego, OR 97035
Hours
Monday–Friday
8:00am – 4:30pm