Causes of Sciatica
Article featured on News-Medical
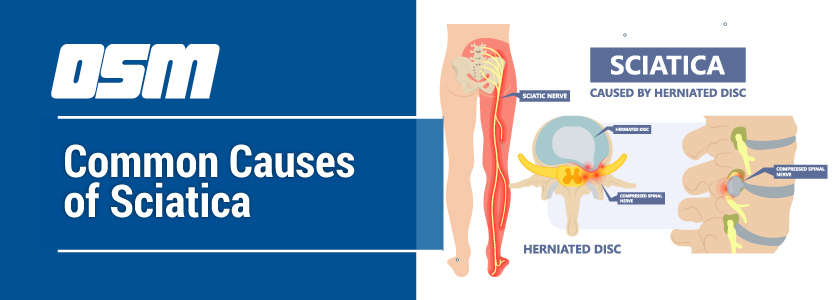
Sciatica is caused by pressure on the sciatic nerve or its roots. Any condition which causes compression of the spinal cord, or the nerve roots emerging from the spinal foramina, causes sensory and motor symptoms in the area supplied by the sciatic nerve in a dermatomal distribution. The most common cause of sciatica is disc herniation in the lumbar region.
The causes of sciatica include:
- Lumbar disc prolapse, or herniation of the cartilaginous intervertebral discs, which then put pressure upon one or more nerve roots in the lumbar region, causing the symptoms of sciatica.
- Lumbar spinal stenosis, or narrowing of the bony canal surrounding the spinal cord, which puts pressure on the lumbar cord and its nerve roots, producing the classic symptoms of compression of the sciatic nerve. Occurring mostly in older people, it is characterized by more or less constant back pain, with leg pain or numbness soon after the patient starts walking.
- Spondylolisthesis, where one disc slips forward over the one beneath, leading to narrowing of the available spinal canal space at that point. This can compress the spinal cord and nerve roots, and in the lumbar region, it causes sciatica. The fourth and fifth lumbar vertebrae are most commonly affected in lumbar spondylolisthesis, which is usually a sequel of spinal arthritis.
- Spinal infection leading to abscess formation in the paraspinal region, causing pressure on the nerve roots or the spinal cord, depending on the location.
- Spinal trauma or injury, leading to deformity which puts pressure on the spinal nerve roots.
- Tumors growing within the spine, which compress the nerve roots.
- Bone spurs or osteophytes, which are outgrowths of bone that form on stressed or degenerating bone, especially following cartilage loss. These can narrow the spinal space, or the space between adjacent vertebra where the nerve roots emerge.
- Piriformis syndrome: the piriformis muscle is a thick small muscle located deep to the large buttock muscles or glutei, and it passes over the sciatic nerve. Spasm, swelling or tightening of this muscle leads to the piriformis syndrome by compressing the nerve. In addition, the nerve passes through the muscle rather than below it in about 14% of people, which may carry a higher risk of sciatic nerve compression.
- Space-occupying lesions in the lumbar region, such as abscesses, clots, tumors, put pressure on lumbar nerve roots or the sciatic nerve itself.
- Poor sitting posture can lead to paraspinal muscle spasm, ligamentary laxity or spinal deformity, putting pressure on the lumbar spine and pinching the nerve roots.
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, foot and ankle conditions, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic and podiatric surgeons in Portland Oregon, contact OSM today.
Phone:
Address
1515 NW 18th Ave, 3rd Floor
Portland, OR 97209
Hours
Monday–Friday
8:00am – 4:30pm