5 Ways for Protecting Your Joints as You Age
Article featured on Orthopaedics of Atlanta and Aesthetic Institute
Every living thing changes as it ages, and the human body is the perfect example. Hair color fades, skin thins and wrinkles, and joints lose lubrication and become arthritic.
Amazing technological advances have made it possible to combat the effects of aging and even reverse it in some cases, but when it comes to your joints, you have the power to prevent the need for medical intervention.
To that end, here are five things you can do now to keep your joints in top shape as you age.
1. Take hydration seriously
More and more people are becoming aware of the importance of hydration and carry a water bottle with them wherever they go, but some still haven’t gotten the message. Did you know that you can live without food for weeks, but you can’t go without water for more than three days?
Children and older adults are at higher risk for dehydration, and it affects multiple body functions, including joints. The cartilage in your joints is 80% water, so when you neglect your water intake, you deplete these tissues, which can lead to joint pain and osteoarthritis.
2. Stop smoking
Smoking is bad for so many reasons, with heart disease and lung cancer at the top of the list. But smoking can also affect your joints.
Nicotine increases inflammation throughout your body, and inflammation means pain. What’s more, smoking constricts your blood vessels, which means your circulatory system can’t work as efficiently at transporting oxygen, and your healing processes become sluggish.
So if you have any joint damage already, smoking may hinder your ability to recover.
3. Don’t skip warmups
In the interest of saving time, you may be tempted to skip the warmup portion of your workout. But if you jump into exercise too quickly, you put yourself at risk for an injury now and joint problems later.
By stretching and moving your muscles before you launch into a full workout, you can prep your joints for what’s to come.
We’re not talking about the old-school stretches where you hold a position for a few seconds. The best way to get your joints ready for action is dynamic stretching, which mimics the types of movements you plan to do in your workout, whether it’s golf, tennis, weightlifting, or running.
Whatever activity you choose, there’s a dynamic stretch to get you ready for it.
4. Lose weight
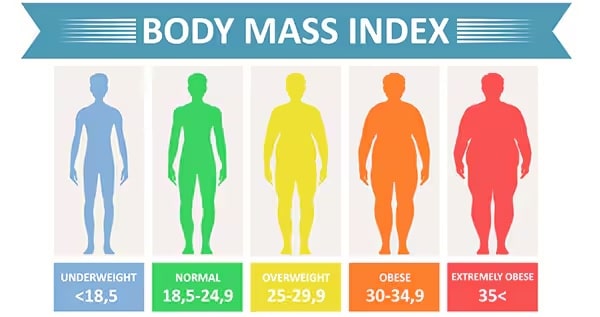
You knew this would make the list. Being overweight or obese increases your risk for just about every health problem, including panful joints. In addition to contributing to inflammation all over your body, making any or all of your joints hurt, extra weight specifically affects your knee joints.
For every pound you’re overweight, you add an extra 4 pounds of pressure on your knees every time you stand, walk, or run. Four pounds may not seem like a lot, but if you’re 30 pounds beyond your ideal BMI, for example, your knees are bearing an extra 120 pound of pressure.
5. Listen to your joints
Aches and pains happen. When you give it your all in a pickup game of basketball, you help a friend move, or you spend the day kneeling in the garden, you can expect to have sore muscles the next day. But joint pain is different. Joint pain differs from muscle pain in that it causes:
- Stiffness
- Redness
- Warmth
- Weakness
- Locking
It’s important to literally listen to your joints, as some conditions can even cause audible symptoms like clicking or popping.
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, foot and ankle conditions, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic and podiatric surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
1515 NW 18th Ave, 3rd Floor
Portland, OR 97209
Hours
Monday–Friday
8:00am – 4:30pm