Does Cold Weather Worsen Arthritis Pain?
Article featured on OrthoNY
Why Weather Affects Arthritis
Approximately 75% of arthritis sufferers believe that weather impacts their symptoms, and many focus on cold temperatures and changes in barometric pressure as the main factors. Others report increasing humidity levels as a contributing factor.
This leads to the question of how cold weather affects arthritis, as well as how do other weather patterns impact this condition?
The Link Between Temperature Changes and Pain Levels
Research into how changes in temperature affect arthritis pain is ongoing. One study revealed that patients’ pain levels increase with every 10-degree decrease in temperature. This may be driven in part by the physiological changes that occur as temperatures drop. For example, synovial fluid, also commonly called joint fluid, may thicken in cold weather. As this liquid, which helps cushion joints and reduce friction, thickens, it may accumulate and create increasing inflammation and stiffness in the affected area.
Additionally, cold temperatures are linked to slower blood circulation, muscle spasms, and increased sensitivity to pain.
The Link Between Barometric Pressure Changes and Joint Pain
Barometric pressure may have an even more dramatic effect than temperature changes. When the pressure drops, muscles and tendons expand. As the connective tissues surrounding joints expand, it can increase the amount of pressure on the joints themselves, which can raise pain levels.
Additional Factors to Consider
Aside from temperature and pressure, it’s important to keep several other considerations in mind. For instance, when the humidity is higher, the moisture in the air can cause tissue in the body to swell, increasing both stiffness and pain. Additionally, research suggests that the average American gets about 30 minutes less physical activity daily during cold weather. That decrease in activity levels can worsen arthritis symptoms.
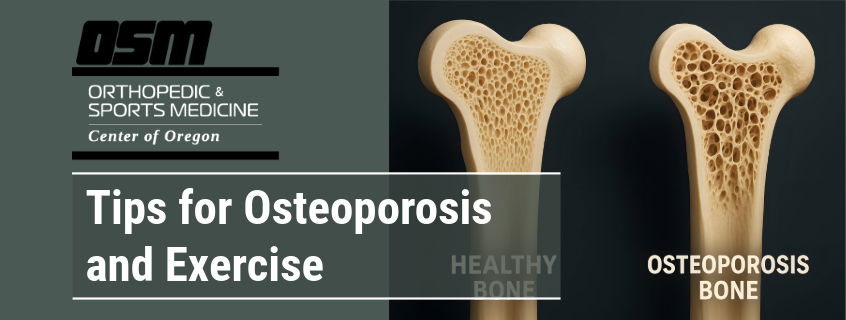
Types of Arthritis Most Sensitive to Cold
Although more than 100 types of arthritis can affect people, two of the most common types, osteoarthritis and rheumatoid arthritis, are linked to increased cold sensitivity. Let’s take a closer look at each type.
Osteoarthritis and Cold Weather
The U.S. Centers for Disease Control estimates that more than 32.5 million Americans have osteoarthritis. Sometimes referred to as “wear and tear” arthritis, this condition is characterized by a breakdown in the cartilage that cushions joints. Cold weather can put further pressure on joints, increasing discomfort and stiffness.
Rheumatoid Arthritis and Cold Weather
This form of arthritis is one of more than 80 different autoimmune disorders. It affects approximately 1.5 million Americans, including 300,000 children. Like other autoimmune conditions, rheumatoid arthritis is caused by the immune system misfiring and attacking the joints and nearby tissues. Cold weather can affect the body’s immune response, which may contribute to worsening symptoms.
Common Cold-Weather Symptoms
For many patients, cold weather increases their existing arthritis symptoms. Whether the affected joints are hips, lower back, feet and ankles, hands and wrists, knees, or shoulders, the symptoms are typically the same. Stiffness, pain, swelling, fatigue, and reduced joint mobility are among the chief complaints.
Cold weather can trigger an arthritis flare-up. In addition to the primary pain symptoms, patients often feel general feelings of being unwell. Additionally, the discomfort and increased inflammation can leave arthritis sufferers feeling drained. That fatigue often leads to many patients lowering their activity levels, which can further worsen symptoms.
Consider practicing preventative strategies, like dressing warmly and staying active before and during changes in the weather.
Managing Arthritis Pain in Cold Weather
Patients working with our providers at any of our Orthopedic Clinic OrthoNY locations receive advice tailored specifically to their conditions and symptoms. Some practical strategies to try include maintaining activity levels, using heat therapy, and eating a diet rich in anti-inflammatory foods.
Low-Impact Exercise
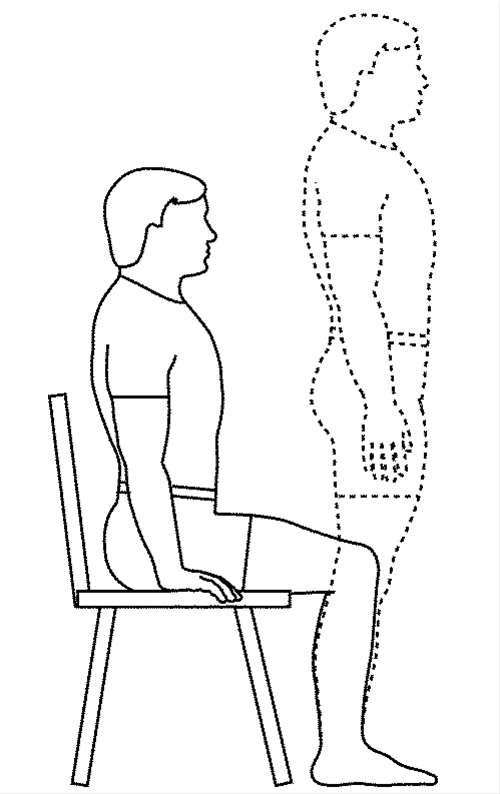
When it’s cold outside and when patients experience discomfort, many opt to take it easy and decrease their activity levels. On average, more than 50% of adults in the U.S. are less active in winter, but for arthritis patients, this can worsen the problem. Increasing movement and keeping up with physical activity can help improve joint flexibility, boost muscle strength, and increase mobility.
A few options to consider include walking, biking, and engaging in water aerobics or swimming. Stretching, yoga, light weight training, and range of motion exercises like knee extensions and arm raises can also be helpful.
Heat Therapy
Dressing warmly can help protect the joints from the cold. Applying heat therapy, like a warm compress, bath, or a heating pad, may help. Heat dilates blood vessels, helping to ward off stiffness and pain. It works by allowing the circulatory system to deliver more nutrients and oxygen to the affected tissues.
Anti-Inflammatory Foods
Many medical professionals recognize the value of incorporating anti-inflammatory foods into the diet to reduce inflammation and help combat symptoms. Eating salmon, sardines, and other fatty fish; leafy greens, such as spinach and kale; and fruits like strawberries, cherries, and blueberries, can help fight inflammation. Olive oil, tomatoes, and nuts also typically top the list of anti-inflammatory foods.
Other foods may offer specific advantages. For example:
- Cruciferous vegetables: Broccoli, cauliflower, and Brussels sprouts contain sulforaphane, a powerful compound shown to slow inflammatory processes.
- Garlic: Along with shallots and onions, this zesty ingredient contains diallyl disulfide, a compound that may help reduce the enzymes that damage cartilage.
- Vitamin-C-Rich Foods: Kiwi, citrus fruit, bell peppers, and cantaloupe all contain vitamin C, a vitamin essential for supporting healthy muscle tissues, blood vessels, and cartilage.
Physical Therapy and At-Home Care
Research suggests that physical therapy can aid in chronic pain management, with a success rate averaging 68% to 72%. Additionally, nearly eight out of 10 patients experience significant pain relief after completing their treatments. OrthoNY provides personalized physical therapy care across the region to help patients combat joint discomfort and regain mobility.
Physical therapists often give patients a list of exercises to do at home. A few exercises to try now include gentle stretching, aquatic therapy, and strength exercises.
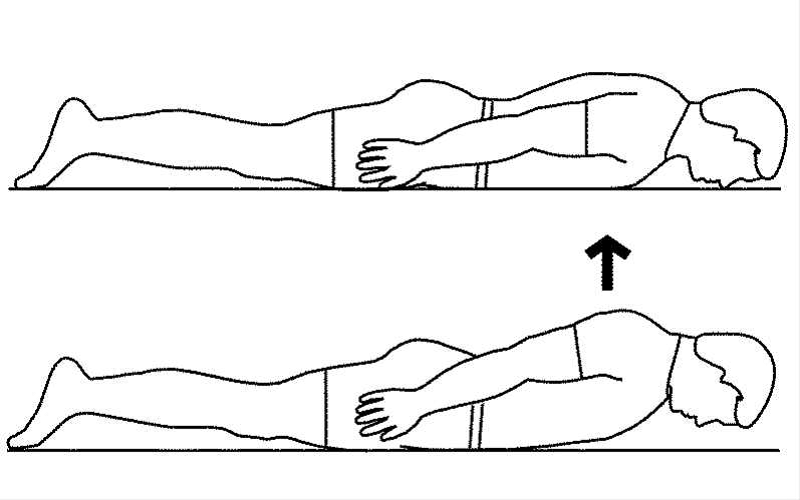
Gentle Stretching
Stretching helps enhance the range of motion and lubricate joints. To get the most out of a session, be sure to warm up with a light walk or gentle movements to get the blood flowing.
A few stretches to try include:
- Knee-to-Chest: Lie on your back on the floor. Bend both knees, placing your feet flat on the floor. Bring your left knee to your chest, grasping it on either side as you pull. Hold it for 30 seconds and release, repeating on the other side.
- Posterior Shoulder and Back: Stand straight and place your arms at your sides. Slowly bring your left arm across your chest. Keep the left arm straight and grasp it at the elbow with your right hand, gently deepening the stretch. Hold it for 30 seconds before returning to the neutral position. Repeat on the right.
- Towel Squeeze: Stretch your hand by grabbing a rolled-up hand towel or a large sponge in your left hand. Squeeze and hold it for five seconds before relaxing and repeating with your right hand.
Aquatic Therapy
Aquatic therapies encompass several activities, including water exercises, which are low-impact and can help boost physical function while lowering pain levels. Water immersion therapy, which involves spending at least 20 minutes in a warm bath, can also be beneficial. A more portable option, heated compresses, can also help ease joint stiffness and soothe aches. These therapies all help improve blood circulation, enhancing your body’s ability to repair damaged tissues. They also enhance relaxation, which can have a beneficial impact on pain and stress.
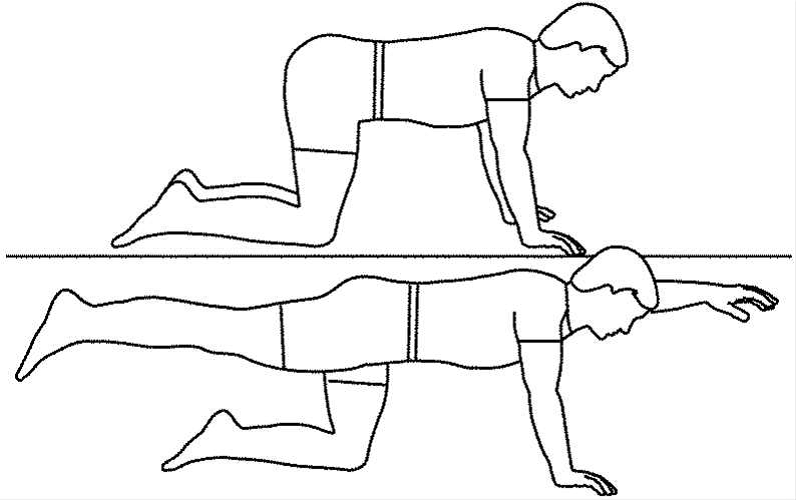
Strength Exercises
These exercises help make muscles, bones, and joints stronger, while also helping to fight fatigue and inflammation. It’s important to start slowly, increasing the intensity by only 10% to 20% when ready. Start with light weights or resistance bands and go slowly to avoid overdoing it. Patients should work with a physical therapist throughout this process. This ensures they follow a strength training routine that will work best for their strengths and limitations and avoid potential injuries.
The Orthopedic & Sports Medicine Center of Oregon
The Orthopedic & Sports Medicine Center of Oregon (OSM) is an award-winning, board-certified orthopedic and sports medicine practice serving Lake Oswego, Portland, Scappoose, and surrounding Oregon communities. Our main clinic is located in Lake Oswego, with additional locations in Portland and Scappoose.
OSM provides comprehensive orthopedic care, sports medicine, spine care, joint replacement, foot and ankle surgery, hand and upper extremity care, and fracture treatment. Our physicians treat a wide range of conditions including sports injuries, arthritis, joint pain, spine conditions, ligament and tendon injuries, fractures, and degenerative musculoskeletal disorders using both surgical and nonsurgical approaches.
Our mission is to help patients return to pain-free movement, strength, and function through personalized treatment plans and advanced orthopedic techniques.
OSM Locations
Lake Oswego (Main Clinic)
17355 Lower Boones Ferry Rd, Suite 100A
Lake Oswego, OR 97035
Portland
5050 NE Hoyt St, Suite 668
Portland, OR 97213
Scappoose
51385 SW Old Portland Rd, Suite A
Scappoose, OR 97056
Phone: 503-224-8399
Hours: Mon–Thurs, 8:00am–4:30pm/ Friday 8:00am–1:00pm
If you are looking for experienced orthopedic surgeons, sports medicine specialists, spine doctors, or foot and ankle experts in Lake Oswego, Portland, or Scappoose, contact The Orthopedic & Sports Medicine Center of Oregon today.