Joint & Bone Health: Injury Prevention Tips
Article featured on Bowen Hefley Orthopedics
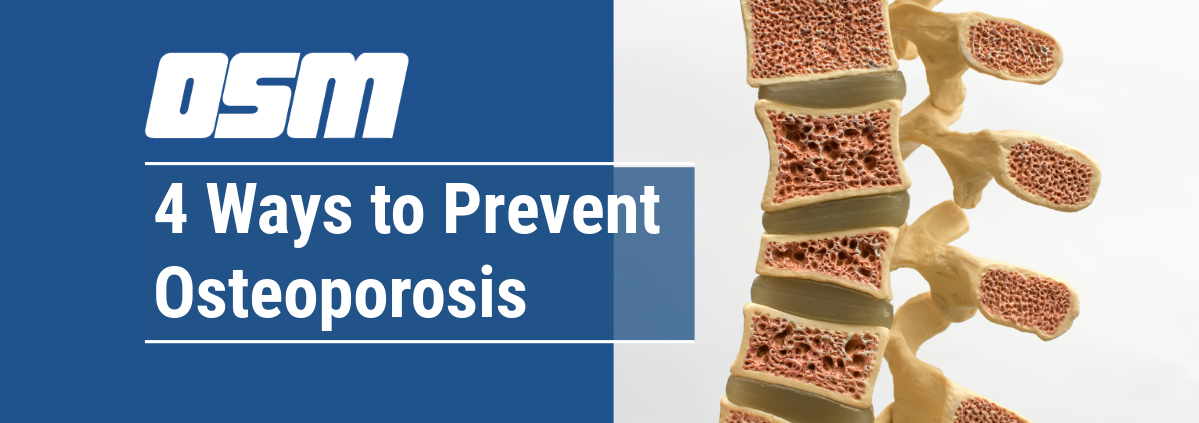
Injuries can have a significant impact on bone and joint health. If you have a bone fracture or torn ligaments or tendons, your musculoskeletal health is severely compromised. There are physical limitations to be expected from such injuries, such as the individual being unable to perform daily activities normally.
Orthopedic doctors always highlight the importance of prevention against orthopedic injuries. From the pain symptoms to possible long-term consequences, injury prevention should be part of your health routine.
Here are some useful tips for preventing orthopedic injuries and maintaining joint and bone health.
#1 Warm Up and Cool Down Before and After Physical Activity
One of the most crucial steps in preventing sports injuries is properly warming up and cooling down before and after physical activity.
- Warming up with exercises like jumping jacks raises your heart rate and body temperature, making your muscles more flexible and less prone to injury.
- Cooling down allows your body to gradually return to a resting state, preventing issues like blood pooling and cramping.
#2 Make Stretching a Daily Habit
Regular stretching increases the range of motion, flexibility, and muscle blood flow. It’s important to stretch all major muscle groups at least two to three times per week. Use dynamic stretching exercises to warm up before the activity and static stretching exercises to cool down afterward.
#3 Use the Right Protective Equipment
Athletes should use the right protective gear for their sport. Here is a list of common protective gear for various sports:
- Helmet: Protects the head and brain in sports like football and hockey.
- Mouthguard: Protects the teeth, gums, and jaw in contact sports such as football and boxing.
- Shoulder Pads: Provides protection for the shoulders, chest, and upper back in sports like football and hockey.
- Elbow Pads: Protects the elbows in sports like hockey and volleyball.
- Knee Pads: Offers protection for the knees during activities like basketball and volleyball.
- Shin Guards: Protect the lower legs, shins, and ankles in sports such as soccer and field hockey.
- Chest Protector: Provides protection for the chest and torso in sports like baseball and softball.
- Gloves: Protects the hands and fingers in sports like hockey and baseball.
- Protective Eyewear/Goggles: Shields the eyes from impact or injury in sports like skiing.
- Protective Cup/Jockstrap: Protects the genitals and pelvic area in contact sports like football and hockey.
Make sure the protective gear fits you correctly to provide adequate protection without limiting movement.
#4 Prioritize Hydration
Proper hydration is essential for all athletes, especially in hot weather. Follow the guidelines recommended by the American College of Sports Medicine (ACSM):
- Drink 17-20 ounces of water two to three hours before exercise
- Drink 7-10 ounces every 10 to 20 minutes during exercise
#5 Don’t Slack on Strength Training
Building strong muscles supports joints and helps prevent injuries, particularly in knee areas. The American Orthopaedic Society for Sports Medicine (AOSSM) recommends strength training sessions targeting the upper body and lower body twice to thrice weekly, focusing on core, leg, and arm exercises.
#6 Avoid Overdoing It
Overtraining can lead to overuse injuries. Gradually increase the intensity and duration of your workouts instead of pushing your body too hard, too fast. This approach helps prevent overuse injuries like stress fractures and plantar fasciitis. If you’re new to exercise, start with 20-30 minutes of moderate activity several times per week.
#7 Use Proper Form
Using proper form during physical activity reduces stress on muscles and joints, minimizing the risk of sports injuries. When lifting weights, choose a weight that allows you to maintain good form comfortably. If you’re unsure about proper technique, consult a certified personal trainer or coach for guidance.
#8 See a Sports Medicine Doctor
These specialized physicians have the expertise to diagnose and treat sports-related injuries and provide preventive care. They can provide individualized recommendations for injury prevention and training programs to enhance athletic performance and strengthen bones and joints.
The Orthopedic & Sports Medicine Center of Oregon
The Orthopedic & Sports Medicine Center of Oregon (OSM) is an award-winning, board-certified orthopedic and sports medicine practice serving Lake Oswego, Portland, Scappoose, and surrounding Oregon communities. Our main clinic is located in Lake Oswego, with additional locations in Portland and Scappoose.
OSM provides comprehensive orthopedic care, sports medicine, spine care, joint replacement, foot and ankle surgery, hand and upper extremity care, and fracture treatment. Our physicians treat a wide range of conditions including sports injuries, arthritis, joint pain, spine conditions, ligament and tendon injuries, fractures, and degenerative musculoskeletal disorders using both surgical and nonsurgical approaches.
Our mission is to help patients return to pain-free movement, strength, and function through personalized treatment plans and advanced orthopedic techniques.
OSM Locations
Lake Oswego (Main Clinic)
17355 Lower Boones Ferry Rd, Suite 100A
Lake Oswego, OR 97035
Portland
5050 NE Hoyt St, Suite 668
Portland, OR 97213
Scappoose
51385 SW Old Portland Rd, Suite A
Scappoose, OR 97056
Phone: 503-224-8399
Hours: Mon–Thurs, 8:00am–4:30pm/ Friday 8:00am–1:00pm
If you are looking for experienced orthopedic surgeons, sports medicine specialists, spine doctors, or foot and ankle experts in Lake Oswego, Portland, or Scappoose, contact The Orthopedic & Sports Medicine Center of Oregon today.