How to Prevent Back Pain When You’re Traveling
Article featured on HealthPartners
1. Motion is lotion for your body! Even when traveling, it’s important to stay active to prevent back pain.
- Use the 30-minute rule.
If you are sitting or standing for 30 minutes, change position. Even if it is only a brief change, it can help prevent back pain. Really, I promise, your back will thank you in the long run.
- Take regular stretch breaks.
Back pain from driving is common. Stop every 60-90 minutes to get out and walk around while traveling by car, or get out of your plane seat and walk the aisle if permitted.
- Do simple exercises while seated to help keep your back from getting stiff.
You can do something called a pelvic tilt while sitting on a plane or in the car to mimic the sit-to-stand motion.
2. Stress can contribute to the intensity of low back pain. The better you can manage stress, the better you can prevent back pain and the less you will hurt.
- Don’t hesitate to ask for help.
Make things easier on yourself and let those who offer to help do so. If the flight attendants will help you lift your bags to the overhead compartment, let them.
- Plan ahead.
Make a list of everything that needs to get done, and allow extra time to do them all in case things don’t go according to plan. That will make it easier to adjust if something unexpected comes up at the last minute (like, traffic or long security lines). If nothing goes awry, you’ll have extra time to relax!
- Practice deep breathing and other mindfulness techniques.
I recommend giving progressive muscle relaxation exercises a whirl. They can be a less time-intensive alternative to yoga or meditation. And since they can easily be done in an airplane seat, they can be very helpful in counteracting the issues that can come from back pain and flying.
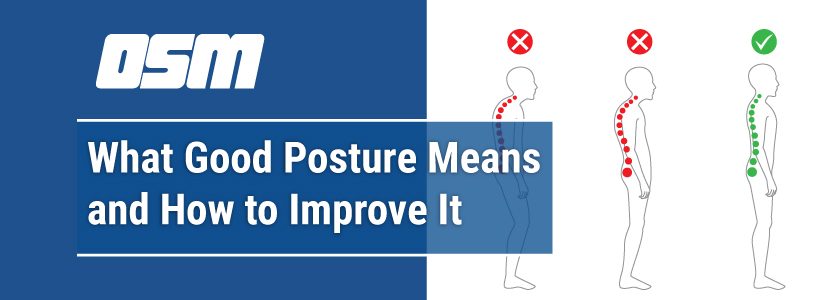
3. There are certain activities that may lead to back pain from driving or flying. So when you’re traveling, make simple changes to what you’re doing to prevent back pain from flaring up.
- When you’re spending a long time in a car or plane…
Use a rolled up towel, sweatshirt, lumbar roll or a water bottle to give your back the proper support it needs for a long trip. Place the object just below the small of your back, above your hips.
- When you’re sleeping in a car or plane…
Use a neck pillow – they really do help. Having a neck pillow will keep your spine in better alignment. And that will decrease the stress that resting in an upright position can put on your neck. If you don’t have a neck pillow, roll up a towel, sweatshirt or small blanket and wrap it around your neck.
- When you’re standing in lines…
Keep your weight equal between both feet, or shift your weight back and forth. When it comes to the issue of back pain and flying, waiting to go through airport security is often a culprit. You can also try propping a foot up on a bag or curb to decrease the stress to your spine.
- When you’re lifting luggage or heavy items off the ground…
Use a wide stance with your feet and squat down using your legs. Keep your butt back and put your weight into your heels.
- When you’re picking small objects off the floor…
Try a technique called the “golfer’s lift.” Kick one leg behind you and bend at the hip like a pendulum, keeping your low back straight. Reach to pick up the object with one arm while using the other to hold a stationary object for support.
- When you’re sleeping in a different bed…
Use blankets to help cushion a hard mattress if you prefer softer surfaces. If you’re lying on your back, prop up pillows under your knees. Or if you’re lying on your side, put a pillow between your knees. This will help you prevent back pain by keeping your spine in a better position.
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
1515 NW 18th Ave, 3rd Floor
Portland, OR 97209
Hours
Monday–Friday
8:00am – 4:30pm