Keeping Your Spine Healthy
Article featured on Brigham Health Hub
While the COVID-19 pandemic has changed our lives dramatically, back and neck problems are still as common as ever. In fact, some people are experiencing pain and other discomforts for the first time due to changes in their work locations and equipment as they moved from the office to home. The good news is that most spine conditions improve with time, physical exercise and getting back to your normal activities.
During the pandemic, Michael W. Groff, MD, a neurosurgeon and the director of the Neurosurgical Spine Service at Brigham and Women’s Hospital, had a virtual visit with a patient who was having neck pain along with tingling and weakness in an arm. The patient had undergone a previous surgery with Dr. Groff and feared he might need another.
While an MRI showed more wear and tear in the man’s neck, Dr. Groff reassured his patient that the condition would likely improve without surgery. The best course of action included physical therapy and performing exercises at home.
“I’m not one hundred percent certain that this patient won’t need surgery again,” says Dr. Groff. “But I reassured him that the path to recovery was to get moving and return to his normal routine. And neither of these things would further hurt his neck.”
Dr. Groff is co-chair for the editorial board of Journal of Neurosurgery: Spine. In this role, he and others have been distributing timely information about providing safe care for spine patients during the pandemic.
Keep your back and neck strong with an exercise routine
To keep your back and neck healthy, Dr. Groff urges his patients to perform any physical activity that helps maintain fitness, strengthens the core muscles and includes stretching. If you have back issues, the best way to stay healthy is to stretch often and keep your core strong.
Many people have found virtual exercise classes or routines that include Pilates, yoga or cardio workouts. To stay in shape, you can also use elastic bands, hand weights and/or perform isometric exercises, like planks or squats at home.
“It’s especially important to avoid being sedentary for long periods of time,” says Dr. Groff. “Being inactive can cause muscles that support the spine to weaken. This can sometimes lead to back or neck pain or exacerbate an existing spine condition.”
Getting regular exercise can have other benefits, too. It can give your day structure and help break up the monotony of staying at home for an extended time. Physical exercise can also help you maintain a positive outlook while navigating this challenging period.
When to seek care for back or neck problems
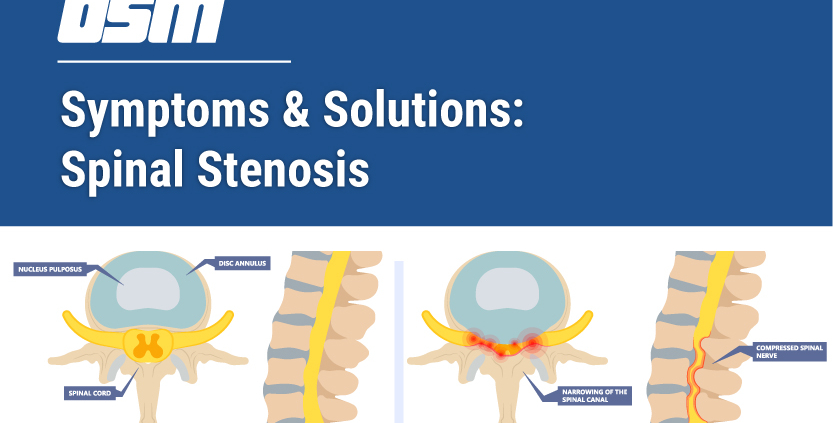
If you have an acute injury, like a pulled back or neck muscle, your pain will likely only last a few days. However, if your symptoms last 2 to 3 weeks and you have weakness or tingling in an arm or leg, contact your doctor.
For pain relief, Dr. Groff recommends ice for the first 48 hours and then alternating between heat and ice for several days after. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), can also help reduce pain and lower inflammation.
For flare-ups of back or neck pain, most spine care providers recommend only staying in bed for about 3 days. In the past, doctors used to recommend a few weeks of bedrest for flare-ups until a pivotal 2016 study showed that 3 days of bed rest is all patients need before they should return to normal activity.
“Staying in bed any longer than 3 days may lead to muscle weakening that can actually worsen a pain episode,” says Dr. Groff. “If you’re having pain, I usually recommend that patients rest and recover over a long weekend and then resume their normal activities.”
Back or neck pain usually doesn’t cause physical damage
If you have back or neck pain, how you interpret it can often impact how disabling it can become. Many patients ask Dr. Groff whether their pain is “all in their heads.” It is, he says, because all pain is experienced in our minds.
“If you’re in pain, most patients find it helpful to know that their pain is most likely not causing physical damage to their spines,” says Dr. Groff. “If you know you aren’t hurting yourself, you can feel better about exercising and returning to your routines.”
Dr. Groff hopes to help patients understand their pain from this new perspective. Doing so often removes the fear of physical activity, because getting back to normal life is a common pathway out of pain for many patients.
“The experience I’ve gained during the COVID-19 pandemic gives me the confidence to say that the Brigham is providing care that’s compassionate, technically excellent and safe for you and your family,” says Dr. Groff.
Dr. Groff can see patients both in person and through virtual visits, which allow him to stay in contact with patients who prefer to connect from home.
“I can still meet with patients and discuss their symptoms during virtual visits,” says Dr. Groff. “I can review imaging and develop a care plan that’s tailored to their unique circumstances. I can also follow up with patients to see how they’re progressing.”
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
1515 NW 18th Ave, 3rd Floor
Portland, OR 97209
Hours
Monday–Friday




 From
From