Hip-Spine Syndrome: It’s Complicated (and Often Overlooked)
Article featured on Brigham Health Hub
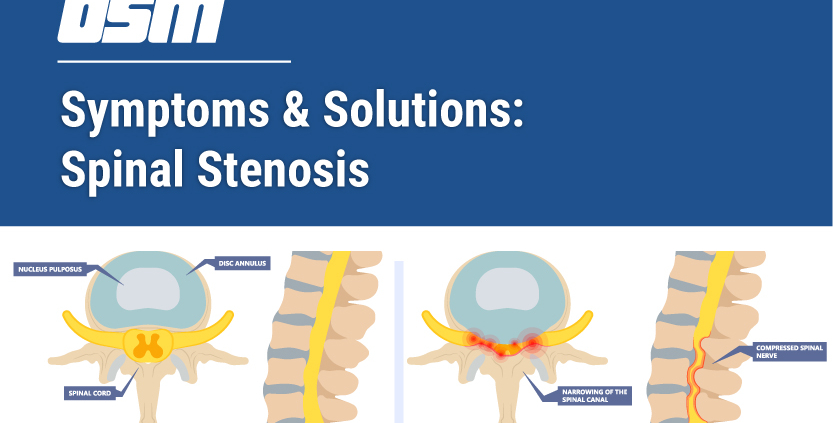
A patient with hip arthritis may experience hip or groin pain as well as trouble walking, while a patient with lumbar spinal stenosis may have pain down their leg, or neurologic symptoms such as numbness, tingling, or weakness.
“Hip-spine syndrome is a distinct syndrome where both hip and spinal problems are occurring together,” says James D. Kang, MD, Chairman of the Department of Orthopaedic Surgery at Brigham and Women’s Hospital.
And yet, because hip and spine disorders have overlapping presentations and symptoms, it can often be challenging for physicians to determine if a patient’s symptoms originate from the hip, spine, or both. This can delay diagnosis and treatment, and many patients with hip-spine syndrome have seen several physicians and therapists or may have undergone various procedures that did not relieve their pain.
“The first order of business is to make sure that the treating physician considers hip-spine syndrome in their evaluation. The problem is that many centers are so sub-specialized that hip surgeons only see hip problems, and spine surgeons only see spine problems,” says Dr. Kang.
“Our department is at the forefront of public awareness and academic awareness of this complicated syndrome. We are spearheading several efforts in orthopaedic research, including clinical investigations and patient outcome studies, trying to determine the optimal treatment plans for patients with hip-spine syndrome,” says Dr. Kang.
For patients with minor hip or back pain, Dr. Kang typically prescribes rehabilitation and physical therapy. Only patients with more advanced hip-spine syndrome who do not respond to physical therapy require invasive treatments, such as an injection therapy, or surgery.
Dr. Kang also recommends lifestyle changes to those with hip and spinal disorders, including weight reduction through diet and exercise. Since many patients with hip-spine syndrome have trouble walking or running, he recommends less active forms of aerobic conditioning, such as swimming and stationary biking.
For those with low back problems quitting smoking is also important, as prolonged exposure to cigarettes has been shown to impair oxygen delivery to tissues, and may cause damage to vascular structures of the discs and joints. Using anti-inflammatory medications can also help modulate symptoms.
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
17355 Lower Boones Ferry Rd Suite 100A
Lake Oswego, OR 97035
Hours
Monday–Friday
8:00am – 4:30pm