5 Causes of Thumb Pain
Article featured on American Society for Surgery on the Hand
The thumb is involved in about 50% of all hand functions. When the thumb is painful or injured, it becomes very difficult to use the hand. During normal life, we take our thumbs for granted. When the thumb is not working properly, tasks are more difficult, and we then realize how important the thumb is. There are several causes of thumb pain including:
- Trigger thumb
- Arthritis
- Tendonitis
- Carpal tunnel syndrome
- Skier’s thumb.
Read below to learn more.
1. Trigger thumb
The tendon that bends or flexes the thumb is called the flexor pollicis longus (FPL). If there is swelling or inflammation around the thumb tendon, it will not glide smoothly. Sometimes the tendon gets stuck in the thumb pulley, causing the thumb joint to click, catch, or lock. This is called a trigger thumb. The thumb can also become swollen, stiff, and very painful. Treatment includes rest, anti-inflammatory medications, splinting, and steroid injections. Most patients improve without surgery. If symptoms persist with treatment, trigger thumb release surgery is very effective and has low risks.
2. Thumb arthritis
The human thumb is unique. We can touch the tip of the thumb to the small finger — a function called opposition. Most animals do not have an “opposable” thumb. This gives us the ability to write, use a needle and thread, and use hand tools. The joint at the base of the thumb which allows opposition is called the carpometacarpal (CMC) joint. Normal, every day activities can cause wear and tear in the thumb CMC joint. When the joint wears out, it can become inflamed and painful. This process is called osteoarthritis or degenerative joint disease.
Anyone can get osteoarthritis if they live long enough. So far, we have not found a way to prevent osteoarthritis. Wear and tear is part of the normal aging process. However, the symptoms of osteoarthritis can be treated by reducing inflammation in the joint. Ways to reduce inflammation and treat thumb CMC osteoarthritis include topical anti-inflammatory gels, oral over-the-counter medications, adjusting hand activities, using a thumb splint, and steroid injections. Most patients improve without surgery. If symptoms persist with treatment, thumb CMC surgery can greatly improve quality of life.
3. DeQuervain’s tendonitis
The tendons in the wrist that lift the thumb up are prone to tendonitis. These tendons travel through a tight compartment on the thumb side of the wrist. If there is friction on the tendons, they can become inflamed and very painful. This is classic in young mothers, and is sometimes called mommy’s thumb. Treatment consists of splinting, anti-inflammatory medications, therapy, and steroid injections. DeQuervain’s release surgery is occasionally necessary to resolve this condition.
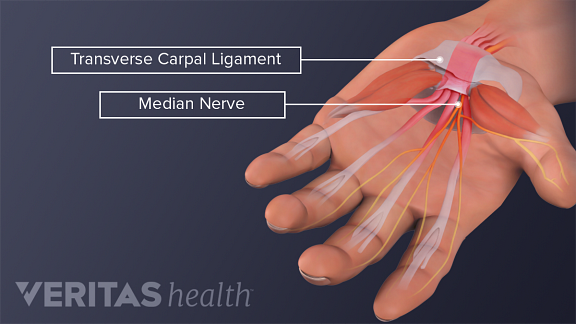
4. Carpal tunnel syndrome
Carpal tunnel syndrome is a type of pinched nerve. When the nerve is pinched in the carpal tunnel, patients have numbness and tingling in the thumb, index, middle, and/or ring fingers. Initially symptoms come and go, and are often worse at night. Some patients feel electric shock sensations or burning pain in their thumbs. In severe cases, the thumb muscles can become weak and atrophied. Treatment for most patients includes wearing a wrist brace at night, stretching exercises, hand therapy, and steroid injections. Carpal tunnel surgery is very effective for most patients if non-operative treatment is not successful or if nerve compression is severe.
5. Skier’s thumb
Trauma to the thumb is common. During a fall, most people land on an outstretched hand to brace themselves. Unfortunately the ligaments in the thumb can become injured in this way. The ulnar collateral ligament (UCL) of the thumb is vulnerable to tearing as the thumb is bent backwards and away from the hand. If this ligament does not heal properly, patients can have pain and weakness with pinch tasks. For most minor sprains of the thumb, temporary immobilization in a splint or cast is successful to allow healing. If the ulnar collateral ligament is fully torn, however, surgery is usually recommended to fix the injury. Hand therapy is often helpful during the recovery process to regain range of motion and strength.
If you have an injury to your hand or thumb, or pain which does not go away with conservative treatment, make an appointment with a hand specialist to get an accurate diagnosis and good treatment plan.
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
1515 NW 18th Ave, 3rd Floor
Portland, OR 97209
Hours
Monday–Friday
8:00am – 4:30pm