What is a Podiatrist/ Podiatric Surgeon?
A podiatrist is a doctor whose degree is “Doctor of Podiatric Medicine (DPM).” The podiatrist is a specialist in the treatment of foot and ankle problems. Before a DPM degree is conferred, a student must complete four years of medical training after college in all aspects of medicine and surgery with special emphasis on lower extremity conditions. Podiatrists have a three years of residency training in foot and ankle surgery following their four years of specialized medical training. After completing surgical residency training, some podiatrists go on to complete extra Fellowship surgical training focused on more complex lower extremity trauma, reconstruction and foot and ankle deformity correction. Many patients seen by the podiatrist are referred by family practice physicians and other specialists who wish to have their patients treated by a doctor trained specifically in foot and ankle disorders. In addition to their surgical training, podiatrists have extensive training in the non-surgical treatment of foot and ankle problems. There is no other specialty that has as extensive training in these areas as the podiatrist.
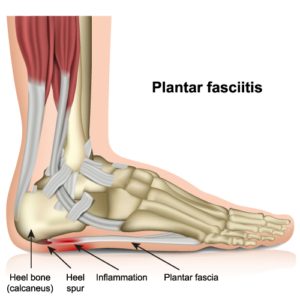
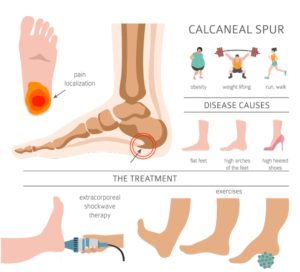
Heel pain, plantar fasciitis, and heel spurs
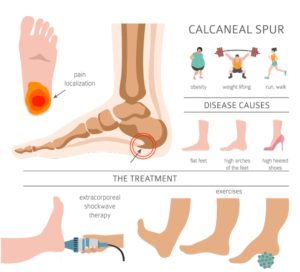 There are a variety of causes of heel pain. Heel pain can occur on the bottom of the heel or the back of the heel. The most common heel pain occurs in the bottom of the heel. Frequently this pain is worse first thing in the morning or after having been at rest. It seems to come out of nowhere or feel like a stone bruise after having been on your feet for long periods of time. Patients often describe the pain as being sharp like stepping on a “spur” or a thorn. The pain may radiate into the arch of the foot or up into the calf muscle. On occasion, leg or foot cramps accompany the condition. Often associated with a spur identified on x-rays, the condition may be referred to as “heel spurs.” A common contributing factor is tightness of the calf muscles.
There are a variety of causes of heel pain. Heel pain can occur on the bottom of the heel or the back of the heel. The most common heel pain occurs in the bottom of the heel. Frequently this pain is worse first thing in the morning or after having been at rest. It seems to come out of nowhere or feel like a stone bruise after having been on your feet for long periods of time. Patients often describe the pain as being sharp like stepping on a “spur” or a thorn. The pain may radiate into the arch of the foot or up into the calf muscle. On occasion, leg or foot cramps accompany the condition. Often associated with a spur identified on x-rays, the condition may be referred to as “heel spurs.” A common contributing factor is tightness of the calf muscles.
The pain is caused by the pull of a very strong ligament that attaches into the bottom of the heel and fans out into the ball of the foot. This ligament, called the plantar fascia, acts as a bow string to help support the arch of the foot. It is like woven rope and does not stretch well. When something causes the arch to flatten, the ligament is stretched more than it can, and it pulls on the heel bone, causing pain. We call this plantar fasciitis. This pain often eases after a few steps as the ligament is forced to stretch. In severe cases the ligament can tear or rupture.
 Home remedies should include soaking your feet in Epsom salts and warm water, taking an over-the-counter anti-inflammatory, heel cushions or shoe inserts, and calf muscle stretching. Wearing a good supportive shoe is very helpful. Surprisingly, wearing a shoe with a 1″ heel may ease the pain.
Home remedies should include soaking your feet in Epsom salts and warm water, taking an over-the-counter anti-inflammatory, heel cushions or shoe inserts, and calf muscle stretching. Wearing a good supportive shoe is very helpful. Surprisingly, wearing a shoe with a 1″ heel may ease the pain.
When seeking professional help, expect to have an x-ray taken to assist in the diagnosis. Treatment is tailored to the patient. Treatment may include a prescription anti-inflammatory drug, a cortisone injection, orthopedic taping of the foot to support the arch,or perhaps custom-made insoles for your shoes called orthotics. When conservative treatment fails, an operative procedure may be required.
Bunions
 A bunion is a deviation of the long bone behind the big toe producing a bump on the side of the foot. Bunions can occur on one or both feet. They tend to be hereditary but can occur without a family history. They are not caused by shoes but are often aggravated by shoe gear. Abnormal movement of the joints just below the ankle joint causes the deformity. This results in the front portion of the foot splaying or widening. As a result the big toe starts to drift toward the second toe and the long bone behind the big toe starts to drift outward. This deformity gradually gets worse with time, making it more painful and difficult to wear shoes. Because the bunion deformity is progressive, it should be evaluated early. Treatment options range from a recommendation on shoes, and possibly inserts for shoes called orthotics, which are used to control the cause of the bunion and halt its progression. In many instances surgery is recommended.
A bunion is a deviation of the long bone behind the big toe producing a bump on the side of the foot. Bunions can occur on one or both feet. They tend to be hereditary but can occur without a family history. They are not caused by shoes but are often aggravated by shoe gear. Abnormal movement of the joints just below the ankle joint causes the deformity. This results in the front portion of the foot splaying or widening. As a result the big toe starts to drift toward the second toe and the long bone behind the big toe starts to drift outward. This deformity gradually gets worse with time, making it more painful and difficult to wear shoes. Because the bunion deformity is progressive, it should be evaluated early. Treatment options range from a recommendation on shoes, and possibly inserts for shoes called orthotics, which are used to control the cause of the bunion and halt its progression. In many instances surgery is recommended.
Our recommendations are based upon the pain associated with the bunion, the patient’s lifestyle, and the degree of the deformity. As the bunion worsens, it becomes more difficult to treat surgically and the healing time is often increased significantly. Over time, the joint in the big toe can become arthritic, lose its flexibility, and become painful with nearly every step. At this stage the surgical treatments are limited, and a joint replacement may be required.
The selection of the procedure to be used is based upon the degree of the deformity, the underlying biomechanical cause of the bunion, and the procedure that will get the patient back to activity in the shortest period of time. There are no magic procedures and no shortcuts to healing time. Your safety and the final satisfactory outcome of your surgery are paramount to us. If you have further questions, please make an appointment for consultation.
High arch and low arch feet
 Pes cavous and pes planus are the scientific terms that describe high arch feet and low arch or “flat” feet. As Podiatrists, we are very interested not only in structure but also in function of the feet. While very few people have 20-20 vision, it is also true that very few people have perfect arch structure. High and low arch feet are just the two ends of the spectrum of foot structure. The more deviation from what is considered perfect, the worse the function becomes. We describe deviation from “the ideal” as imbalance in structure. It is the imbalance in structure that leads to abnormal function. Abnormal function causes pain and/or deformity. Deformity can manifest itself in a variety of foot problems such as bunions or hammertoes. Likewise, pain can manifest itself in a variety of ways such as heel pain (plantar fasciitis or heel spur), corns or calluses, metatarsalgia or pain in the ball of the foot (neuromas, stress fractures, or tendonitis), or even in pediatric problems.
Pes cavous and pes planus are the scientific terms that describe high arch feet and low arch or “flat” feet. As Podiatrists, we are very interested not only in structure but also in function of the feet. While very few people have 20-20 vision, it is also true that very few people have perfect arch structure. High and low arch feet are just the two ends of the spectrum of foot structure. The more deviation from what is considered perfect, the worse the function becomes. We describe deviation from “the ideal” as imbalance in structure. It is the imbalance in structure that leads to abnormal function. Abnormal function causes pain and/or deformity. Deformity can manifest itself in a variety of foot problems such as bunions or hammertoes. Likewise, pain can manifest itself in a variety of ways such as heel pain (plantar fasciitis or heel spur), corns or calluses, metatarsalgia or pain in the ball of the foot (neuromas, stress fractures, or tendonitis), or even in pediatric problems.
Invariably, we treat almost all foot imbalance or biomechanical insufficiencies with orthotic therapy.
Corns, calluses, and warts
Corns, calluses and warts are areas of thickened skin irritations that can occur on the foot. Calluses are thick, painful skin irritations that can occur on the bottom of the foot. If the thickened area is on top of the toes, we call it a corn. Corns are usually caused by shoes pressing against the toes. They are made worse if the toe is crooked or contracted (hammertoe). These areas generally represent areas of excessive pressure or friction in shoes or while walking on hard surfaces. Caution should be used whenever using any type of corn or callus removers because these medications contain acids that burn the thickened skin off. If you have diabetes, you should never use these medications without a physician’s guidance. These irritations will generally reoccur after use of these medications because the source of irritation is still present. Home remedies might include shoe cushions or pads, and if they are between the toes, cotton or pads might be used. Warm water soaks and then buffing with a pumice stone may help. Creams and lotions may be of some temporary help.
Warts are hard areas that most often occur on the bottom of the foot and are called plantar warts. The bottom of the foot is called the plantar aspect of the foot, thus the name plantar warts. Plantar warts are caused by a viral infection of the skin. They do not have roots or seeds, they only live within the full thickness of the skin. Because a virus causes them, they can spread. They are not highly contagious, but will often spread to other areas of the foot. If you have plantar warts, do not pick at them and do not share your shoes with others. There are over-the-counter wart removers. They generally do not work because the skin is so thick, and it is difficult for the medicine, which is an acid, to penetrate to the depth necessary to kill the wart. Warts can be difficult to treat even for your doctor. Some can be quite persistent; so, it is best to catch them early and get treatment before they become established.
Bone spurs
Bone spurs may occur anywhere a muscle, tendon or ligament attaches to a bone. Generally a spur will only be painful if it causes pressure to some other surrounding structure. Common areas of bone spurs in the foot are in the toes, the heel, the big toe joint, the top of the foot, and the ankle. The location of the spur and the amount of discomfort determines what the doctor recommends for treatment. This may consist of something as simple as a pad or cushion, a cortisone injection, or even surgery to permanently solve the problem.
Ingrown and fungal toenails
Ingrown toenails are quite common in all age groups. Patients often live with them needlessly for months or years. The improper trimming of the nails, tight shoes, or injury to the nail can cause ingrown toenails. Often they seem to occur for no reason at all. If they become infected, you should soak them in warm water and Epsom salts, apply an antibiotic ointment and make an appointment to have them treated. Treatment is virtually painless. Following the procedure there is little to no pain and no limitation of your activities once the anesthesia has worn off.
Fungal toenails are toenails that have become infected with one of a group of microorganisms we call fungus. In many instances it is the same organism that causes athlete’s foot. As the fungus invades the nail and the nail bed, it may go unnoticed for a period of time because it is rarely painful. It usually appears at the nail edge and works its way under the nail, progressing back to the root of the toenail. Once it invades the root, or matrix, it begins to distort the way the nail grows and becomes more difficult to treat.
In early stages, clipping the diseased portion of the nail away and applying an antifungal cream after drying the toe can treat the problem. In later stages of the disease, oral medications may be useful with or without nail removal.
Metatarsalgia-neuromas, stress fractures, and tendonitis
A pain experienced in the ball of the foot may have several different origins: stress fractures, neuromas, or tendonitis.
A stress fracture often begins either gradually or abruptly and is accompanied by swelling and occasionally some discoloration.
Pain that is intermittent or sharp and radiates into the toes may be a neuroma. A neuroma is a swollen nerve that gets pinched between the long bones behind the toes. It has often been described as a nerve tumor; however, in the strictest sense it is not a tumor but rather a swelling of the nerve secondary to some form of irritation. If left untreated the symptoms will often worsen.
Tendonitis is an inflammation in the ball of the foot associated with the tendons that go into the toes. The symptoms are similar to those associated with the neuroma. Tendonitis is often seen in runners and in women who wear high heeled shoes.
Home remedies for all of these conditions consist of wearing stiff-soled shoes with plenty of room in the toe area; over-the-counter anti-inflammatories such as Advil, Tylenol, Motrin or Alieve; and foot soaks in warm water and Epsom salts.
Hammertoes
A hammertoe is a term used to describe a crooked, deviated, or contracted toe. Contrary to popular belief, hammertoes are usually not caused by ill or tight fitting shoe gear but by an imbalance in the way the bones of the foot are aligned. Over a period of years, the tendons that move the toe up and down begin to pull the toe with unequal tension, and the toe then begins to buckle or become contracted. Normally hammertoes by themselves are not painful, but with shoe gear the prominent knuckle of the toe rubs the shoe, producing an area of irritation which eventually forms a corn.
Conservative care may include padding, wider shoes, thicker socks, or even orthotics to try to correct the underlying imbalance. If the problem cannot be managed and produces continual pain, then surgical correction can be accomplished either in the offices or at an outpatient surgical center.
Sports related injuries
Biomechanics is the basis of all lower extremity sports related injuries. The doctors are also members of the American Academy of Podiatric Sports Medicine.
In many instances the treatment of sports related injuries begins with understanding the underlying biomechanics of their cause. There is such an array of these injuries that space does not permit outlining all of them. The more common injuries include shin splints, arch pain, heel pain, Achilles tendonitis, ankle injuries, stress fractures, tendon injuries about the ankle and rear foot, toenail injuries, nerve injuries, and blistering of the skin, to list just a few.
Our advice to all athletes is to incorporate a rigorous stretching program into your workout. The adage of “no pain, no gain” could not be further from the truth. Pain is a warning sign; and if the pain is recurrent and ignored, then the amateur athlete is asking for trouble and, possibly, significant down time from his or her sport or exercise program.
You should choose your athletic shoes with care and be timely in replacing them when they wear out. A good pair of over-the-counter insoles is often useful for minor areas of foot irritation. Following a particularly rigorous workout, areas of soreness are often eased with the use of an over-the-counter anti-inflammatory such as Tylenol, Advil or Aleve. Icing the area can also be useful. If your pain persists, make an appointment and allow us to evaluate your condition and make recommendations for your treatment. Many sports medicine problems are also treated with orthotics.
Diabetes
Diabetic patients are particularly at risk for significant foot problems that can lead to the loss of their feet or legs. The most common cause of hospitalization for the diabetic patient is foot infections. Foot related problems for the diabetic patient are responsible for significant time off work. Foot ulcerations can take weeks or months to heal.
Our physicians are experts in the treatment of diabetic foot disorders, infections, and limb saving techniques. Both doctors are members of the American Diabetes Association and attend regular educational meetings dealing with the treatment of the diabetic’s foot conditions.
There are two conditions that are associated with diabetes that put the patient at risk. The first is called neuropathy, which is a nerve condition that frequently affects the feet. There is a gradual loss in the patient’s ability to perceive the protective sensations. The protective sensations are the ability to feel pain, to feel the difference between hot and cold, sharp and dull, vibration, and excessive pressure. This loss of sensation can become quite profound. Patients can step on sharp objects or cut themselves and not feel pain. They may burn themselves with scalding water and not be aware of it, and they can develop pressure sores and infections and experience little or no pain.
Because of this condition, diabetic patients must be constantly aware of their feet and inspect them daily. They should avoid walking barefoot and always check the temperature of their bath water or foot baths prior to immersing their feet. Special care should be taken when trimming the toenails. The sharp trimming of corns and calluses and over-the-counter corn removers should be avoided. Shoe gear must be appropriately fitted to avoid areas of irritation. Frequently this condition causes a burning pain that makes sleeping difficult. Other patients may feel like their feet are ice cold and have difficulty warming them. These patients must not use heating pads or hot water bottles to warm their feet or they risk burns to the skin that may not heal and could lead to the loss of their foot or leg.
The other condition is called angiopathy, which is the loss of blood circulation to the feet and legs. Loss of circulation results in prolonged healing of cuts or sores on the feet. In severe cases it can lead to gangrene and limb loss. This condition is often accompanied by thinning of the skin, loss of hair growth and color changes to the feet. The feet are cool to the touch and can be very sensitive, making it painful to walk for even short distances.
Of course, the diabetic may have both of these conditions. In this situation, the patient is at significant risk of limb loss and must be monitored very closely.
Common problems the diabetic might encounter are ingrown or fungal toenails, thick calluses on the bottom of the feet, or corns on or between the toes. These relatively simple problems are the precursors of more significant problems. Our recommendation is that diabetic patients have their feet checked on a regular basis by a podiatrist. If they notice any areas of possible skin irritations, sores, or infection, they should be treated professionally by a podiatrist. If they notice a change in the shape of their feet, the arches falling, or notice swelling of sudden onset, they should be seen by a podiatrist. The diabetic patient’s best defense against infections and possible loss of feet or legs is prevention by daily inspection and having regular foot exams.
Pediatric foot problems
Our physicians have extensive training in diagnosing and treating child related foot disorders. Infants and young, growing children have special circumstances that necessitate they be evaluated by a specialist familiar with normal development. Many conditions, if caught early, can be easily treated, correcting the problem before it becomes a life-long deformity. Common foot disorders that we treat include in-toeing and out-toeing, flat feet, curved feet, toe walking, inflamed growth plates in the bones, leg cramps and night cramps, ingrown toenails, athlete’s foot, and other skin conditions. We also treat young athletes and sports related injuries of all ages. Children will often not complain about pain associated with their sport. The demands of soccer, baseball, dance, and gymnastics on the growing child will often uncover underlying developmental problems.
One common myth is that children have “growing pains”. Growth is not painful and soreness and cramping in the feet and legs are not normal. This generally is the result of muscle imbalance or flat feet, which strains the muscles in the feet and legs that are trying to support the foot. A family history of foot problems is significant since many foot problems are hereditary. Often parents are told that their children may “grow out of it.” This may be true in some cases but a level of reassurance from a specialist can go a long way in easing a parents’ concern. If you have concerns about your child’s feet, please make an appointment and let’s discuss your concerns and evaluate your child.
Cortisone injections
Cortisone is a very safe and useful medication. The type of cortisone given is similar to the type of cortisone your body produces naturally. It is useful in halting an ongoing inflammatory process that is impeding your body’s ability to heal itself. It can, in many instances, halt the painful process permanently. In other instances, it is useful in the short-term treatment of pain so additional modalities have a greater opportunity to effect a cure of the problem. Cortisone will not dissolve bone spurs, but it is useful in shrinking swollen and inflamed soft tissues.
If a cortisone injection is suggested and you have concerns, we encourage you to discuss them with us. Our goal is to provide you with the highest quality care. Part of providing that care is ensuring that you are comfortable with the plan and understand the treatment.
What are orthotics?
Orthotics, which are often used in the treatment of biomechanical disorders, are custom molded inserts for shoes that correct foot function and improve efficiency during gait. They are not only useful for the treatment of foot problems but also can be used for the treatment of ankle, knee, hip, and lower back complaints when these disorders have their origin with abnormal foot function and gait.
Why do I need orthotics?
Everyone’s foot structure is different. Just as each individual’s eyesight, personality, and medical problems are unique to that person, so is his foot structure unique. The foot is composed of 26 bones, 107 ligaments, numerous tendons, and 19 muscles originating in the leg and the foot. The way these bones, muscles, and tendons work together determines the balance and alignment of the foot. This, together with your weight, the type of work you do, the amount of time you are on your feet, and the type of surface you stand on all day, not to mention the type of shoes you wear, also contributes to the delicate balance and alignment of your feet. A perfectly balanced and aligned foot is extremely rare.
Practically all foot problems are directly or indirectly related to foot malalignments. If you are experiencing any foot pains, deformities, fatigue, cramps, etc., you probably have an imbalance in your feet. Orthotics are designed to correct or rebalance that abnormality. Just as glasses or contact lenses help to correct your eyesight, orthotics help re-balance your foot structure to reduce abnormal stresses or abnormal areas of weight bearing in your feet that lead to discomfort and that can cause more serious problems as time passes.
What do orthotics look like?
Orthotics look much like supports. There are many types that can be prescribed: some are rigid, some soft and flexible. The doctor will decide which type you need depending on the problems you are having. In all cases, the devices fit in closed shoes and can be transferred from one pair of shoes to another.
How long do I have to wear orthotics?
Depending on your problem, orthotics should be worn the majority of the time you are on your feet, if possible. Once you become accustomed to them, you will probably feel uncomfortable without them. This is not to say that you must wear orthotics when you want to dress up on occasion with shoes that are not compatible with the devices.
What type of shoes are compatible with orthotics?
Most closed shoe with a heel height of 1-1/2″ or less. Orthotics are useless in high heeled shoes and will usually slip out of sandals. Obviously, they can’t be worn when you are barefoot. The most compatible shoe is a closed lace up type of shoe such as an athletic shoe. For women, as the shoe becomes more “dressy” the orthotic may become incompatible. In theses instances, a second pair of “dress orthotics” may be needed.
Can orthotics be used for sports activities, i.e., running, aerobics, etc.?
Definitely! In fact, many professional and amateur athletes treated in this offices would be unable to perform without their orthotics.
Do orthotics ever have to be replaced? Can they break?
If you are an adult, it is not likely that your orthotic prescription will have to be changed. Occasionally your foot structure may change over a period of time and a new prescription may be necessary, but this is rare. In children, new prescriptions may be necessary, and orthotics need to be changed after two to four years of use, and possibly sooner if the child has a growth spurt. Most orthotics will not break depending on the material they are made of, however they are not invulnerable to extreme heat, theft, or the dog chewing them up! Occasionally, they may need to be refurbished when the corner or heal post wear thin.
What is involved in having orthotics made?
A detailed biomechanical evaluation with objective measurements of the joint movements in your feet, ankles, knees, and hips is necessary to prescribe orthotics to fit your individual foot. Occasionally certain muscle groups may also be treated, along with posture, evaluation of pelvic tilt, back problems or malalignments such as scoliosis of the spine. Gait or walking analysis may also be included. This examination, along with angular measurements of the bones of the foot seen in your x-rays, is used to determine a prescription for your orthotics.
We use modern technology to take a 3D scan of your foot, so your orthotics will be 100% specific to your foot.
Ankle Fractures
Ankle fractures are a common injury. Assessment should include looking at the mechanism of injury, comorbidities, associated injuries, soft tissue status and neurovascular status. Emergent reduction is required for clinically deformed ankles. Investigations should include plain radiographs and a computed tomography scan for more complex injuries or those with posterior malleolus involvement. An assessment of ankle stability determines treatment, taking into account comorbidities and preoperative mobility which need special consideration. Non-operative management includes splint or cast, allowing for early weightbearing when the ankle is stable. Operative management includes open reduction and internal fixation, intramedullary nailing (of the fibula and hindfoot) and external fixation. Syndemosis stabilisation includes suture button or screw fixation. The aim of treatment is to restore ankle stability and this article explores the current evidence in best practice.

 There are a variety of causes of heel pain. Heel pain can occur on the bottom of the heel or the back of the heel. The most common heel pain occurs in the bottom of the heel. Frequently this pain is worse first thing in the morning or after having been at rest. It seems to come out of nowhere or feel like a stone bruise after having been on your feet for long periods of time. Patients often describe the pain as being sharp like stepping on a “spur” or a thorn. The pain may radiate into the arch of the foot or up into the calf muscle. On occasion, leg or foot cramps accompany the condition. Often associated with a spur identified on x-rays, the condition may be referred to as “heel spurs.” A common contributing factor is tightness of the calf muscles.
There are a variety of causes of heel pain. Heel pain can occur on the bottom of the heel or the back of the heel. The most common heel pain occurs in the bottom of the heel. Frequently this pain is worse first thing in the morning or after having been at rest. It seems to come out of nowhere or feel like a stone bruise after having been on your feet for long periods of time. Patients often describe the pain as being sharp like stepping on a “spur” or a thorn. The pain may radiate into the arch of the foot or up into the calf muscle. On occasion, leg or foot cramps accompany the condition. Often associated with a spur identified on x-rays, the condition may be referred to as “heel spurs.” A common contributing factor is tightness of the calf muscles.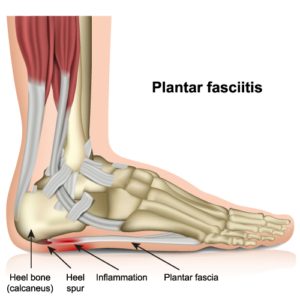 Home remedies should include soaking your feet in Epsom salts and warm water, taking an over-the-counter anti-inflammatory, heel cushions or shoe inserts, and calf muscle stretching. Wearing a good supportive shoe is very helpful. Surprisingly, wearing a shoe with a 1″ heel may ease the pain.
Home remedies should include soaking your feet in Epsom salts and warm water, taking an over-the-counter anti-inflammatory, heel cushions or shoe inserts, and calf muscle stretching. Wearing a good supportive shoe is very helpful. Surprisingly, wearing a shoe with a 1″ heel may ease the pain. A bunion is a deviation of the long bone behind the big toe producing a bump on the side of the foot. Bunions can occur on one or both feet. They tend to be hereditary but can occur without a family history. They are not caused by shoes but are often aggravated by shoe gear. Abnormal movement of the joints just below the ankle joint causes the deformity. This results in the front portion of the foot splaying or widening. As a result the big toe starts to drift toward the second toe and the long bone behind the big toe starts to drift outward. This deformity gradually gets worse with time, making it more painful and difficult to wear shoes. Because the bunion deformity is progressive, it should be evaluated early. Treatment options range from a recommendation on shoes, and possibly inserts for shoes called orthotics, which are used to control the cause of the bunion and halt its progression. In many instances surgery is recommended.
A bunion is a deviation of the long bone behind the big toe producing a bump on the side of the foot. Bunions can occur on one or both feet. They tend to be hereditary but can occur without a family history. They are not caused by shoes but are often aggravated by shoe gear. Abnormal movement of the joints just below the ankle joint causes the deformity. This results in the front portion of the foot splaying or widening. As a result the big toe starts to drift toward the second toe and the long bone behind the big toe starts to drift outward. This deformity gradually gets worse with time, making it more painful and difficult to wear shoes. Because the bunion deformity is progressive, it should be evaluated early. Treatment options range from a recommendation on shoes, and possibly inserts for shoes called orthotics, which are used to control the cause of the bunion and halt its progression. In many instances surgery is recommended. Pes cavous and pes planus are the scientific terms that describe high arch feet and low arch or “flat” feet. As Podiatrists, we are very interested not only in structure but also in function of the feet. While very few people have 20-20 vision, it is also true that very few people have perfect arch structure. High and low arch feet are just the two ends of the spectrum of foot structure. The more deviation from what is considered perfect, the worse the function becomes. We describe deviation from “the ideal” as imbalance in structure. It is the imbalance in structure that leads to abnormal function. Abnormal function causes pain and/or deformity. Deformity can manifest itself in a variety of foot problems such as bunions or hammertoes. Likewise, pain can manifest itself in a variety of ways such as heel pain (plantar fasciitis or heel spur), corns or calluses, metatarsalgia or pain in the ball of the foot (neuromas, stress fractures, or tendonitis), or even in pediatric problems.
Pes cavous and pes planus are the scientific terms that describe high arch feet and low arch or “flat” feet. As Podiatrists, we are very interested not only in structure but also in function of the feet. While very few people have 20-20 vision, it is also true that very few people have perfect arch structure. High and low arch feet are just the two ends of the spectrum of foot structure. The more deviation from what is considered perfect, the worse the function becomes. We describe deviation from “the ideal” as imbalance in structure. It is the imbalance in structure that leads to abnormal function. Abnormal function causes pain and/or deformity. Deformity can manifest itself in a variety of foot problems such as bunions or hammertoes. Likewise, pain can manifest itself in a variety of ways such as heel pain (plantar fasciitis or heel spur), corns or calluses, metatarsalgia or pain in the ball of the foot (neuromas, stress fractures, or tendonitis), or even in pediatric problems.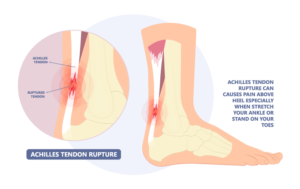
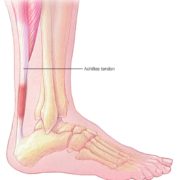 Achilles tendinitis is an overuse injury of the Achilles (uh-KILL-eez) tendon, the band of tissue that connects calf muscles at the back of the lower leg to your heel bone.
Achilles tendinitis is an overuse injury of the Achilles (uh-KILL-eez) tendon, the band of tissue that connects calf muscles at the back of the lower leg to your heel bone.