Understanding Osteoporosis in Women
Osteoporosis is a serious threat to women’s bone health, affecting millions worldwide.
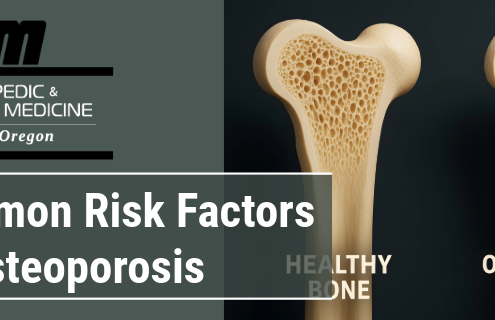
Common Risk Factors of Osteoporosis
Osteoporosis is a bone disease that causes a decrease in bone mineral density and bone mass. Learn about common risk factors.

Joint & Bone Health: Injury Prevention Tips
Injuries can have a significant impact on bone and joint health. If you have a bone fracture or torn ligaments or tendons, your musculoskeletal health is severely compromised. T
10 Tips for Maintaining Bone & Joint Health
When it comes to our health, we often focus on cardiovascular fitness and weight management, but there is another crucial aspect that deserves our attention: bone and joint health. Orthopedic injuries, which involve damage to our musculoskeletal system, can significantly impact our quality of life, limiting mobility and causing persistent pain.
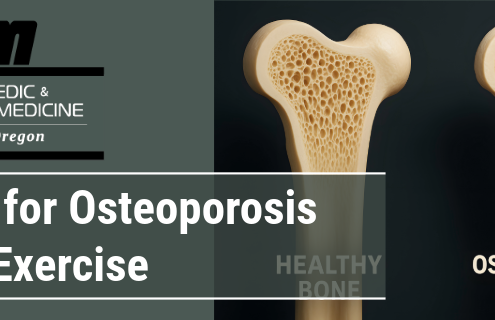
Tips for Osteoporosis and Exercise
You’ve been given the diagnosis of Osteoporosis, learn what exercises are best to improve health and movement with this moving forward.

Exercising and Bone Health
Understand the importance of regular physical activity in building and maintaining healthy bones. Inactivity causes loss of bone!

Bone-Boosting Foods
Poor bone health can cause conditions such as rickets and osteoporosis and increase the risk of breaking a bone from a fall later in life.

Strong Bones at Any Age: A Guide to Lifelong Nutrition
Article featured on National Spine Health Foundation
Nutrition…

Tips to Keeping Your Bones Healthy
Bones do a lot for your body. While it's important to build strong, healthy bones during your childhood and teen years, you can take steps to protect bone health when you're an adult too.

Essential Nutrients Your Body Needs for Building Bone
If you eat a healthy diet (with lots of fruits, vegetables, legumes, nuts, seeds, and lean proteins), you'll get enough of most nutrients needed to keep your bones healthy and functioning well.
