Mending Your Bone Fracture: What Doctors Say
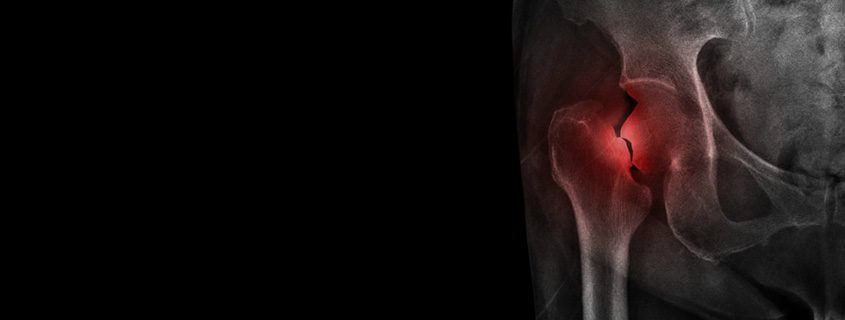
About 6 million people break bones in the United States every year. The most frequently broken bone is the clavicle, or collarbone. Other common bone fractures include those in the arms, wrists and ankles. If you’re over 65, you’re more likely to break your hip than any other bone. You can break bones due to injury or diseases like osteoporosis, which weakens bones. Orthopedic surgeons specialize in treating broken bones in all scenarios. Here’s what three board-certified orthopedists want you to know about bone fractures, risk factors associated with them, and tips for helping them heal properly.
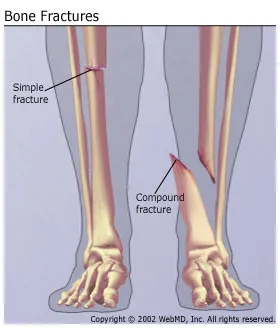
1. “A fracture and a break are the same thing.”
Patients frequently think bone fractures and bone breaks are different. Sometimes people think “fracture” means a crack while “break” means a clearly separated bone, but this is not true. “Fracture” is simply the term doctors use to refer to any break or crack in a bone.
2. “If you smoke, your fracture might not heal as fast.”
If you ingest nicotine—whether through cigarettes, cigars, chew tobacco, or even the nicotine patch—you may find that your fracture takes longer to heal than for a non-smoker. This is due to the effect of nicotine on the healing process. If you quit smoking, it will take three months before your body responds to bone breaks like a non-smoker’s would.
3. “Try RICE for non-emergency injuries.”
If you have a broken bone cutting through your skin or your bones are looking crooked and weird (what doctors call a deformity), you need emergency medical care. But if you only have pain and swelling, and aren’t sure if it’s a break, he says, you could try treating your injury at home for a day or two with “RICE”: rest, ice, compression (wrapping with an ace-type bandage) and elevation. If that doesn’t work, then you can be seen by a doctor.
4. “Don’t wait too long to be seen.”
If you wait too long to bring your possible bone fracture to your doctor’s attention, your bone could start healing on its own—and possibly in a crooked way. That makes fixing the problem more difficult than if you’d come in earlier. Or you could have underlying damage to the surface of the joint or other problems that are harder to treat the longer you wait. Waiting can also make it more likely you’ll need surgery. For non-emergency fractures it is recommended patients be seen within a couple of days. If you require an operation, this gives you time to get it scheduled before bones start knitting back together (which usually happens within a few weeks).
5. “Even little fingers and toes need to be checked out.”
You crack your little toe against a table leg. Should you bother getting it checked for fracture? It depends how bad you feel, noting that in similar situations, he might wait a couple days and, if still in pain, see a doctor to have it X-rayed. But in general, it’s better to err on the side of caution and see your doctor. After all, broken toes that heal crookedly can cause your shoes not to fit right, resulting in pain. Similarly, ignoring finger fractures can cause “significant disability” and lead to longer surgeries once patients finally come in, he says.
6. “Moving it doesn’t mean it is not broken.”
Patients say they didn’t think their bone was broken because they could still move the affected body part. But, he says, this is a fallacy. There’s only one way to know if it’s broken and that’s with an X-ray. The idea that if I can move it, therefore it can’t be broken is ridiculous. You can almost always move it, even if it is broken. Signs that it could be a bone fracture include significant swelling, tenderness around the site, bruising, and an inability to bear weight on it even after a couple of days’ rest.
7. “I don’t always operate.”
People think orthopedic surgeons do surgery 99% of the time. This can cause some patients to avoid seeing them, because they think they’ll wind up in the operating room. It’s perhaps an understandable misconception, given that “surgeon” is part of his title. But, most of what they do isn’t surgery. Instead, orthopedists do the least invasive procedures possible first to promote bone fracture healing, only moving up to surgery if more conservative measures don’t work.
8. “When we tell you to elevate it, take us seriously.”
Folks come in a couple of days after a broken ankle, for example, and they may have been laying around on the couch but not with the ankle truly elevated—which is above the level of your heart. If you’re lying down, you can put two or three pillows under your leg to achieve proper elevation, but if you’re sitting, you’re going to have to use more than that to get your leg high enough. Elevation is key to preventing swelling, which also could delay surgery, if that’s needed.
9. “Splints are not second-class citizens.”
Casts are non-removable and go all around your broken bone, while splints go only halfway around and can be taken off and on. Both casts and splints are used to immobilize your broken bone and both can be written on and decorated. Yet some patients think casts are best and get disappointed if they get a splint instead. A lot of times patients don’t give the splint a lot of respect. Doctors use splints for several reasons, including when a cast is difficult to place due to the location of the break or when doctors want to leave room for swelling.
10. “Forget the ‘6-week rule’ of bone healing.”
Patients think they know fractures are cured in six weeks, which is an incredible piece of misinformation; no adult is going to heal in six weeks. Most bone fractures take anywhere from 2 to 6 months to heal, depending on many factors, he says. There’s not just one rule for every broken bone. It’s important to understand there is specificity and details matter, such as where a bone is broken, what bone it is, what the fracture pattern looks like, and so on. It’s difficult to generalize.
The Orthopedic & Sports Medicine Center of Oregon is an award-winning, board-certified orthopedic group located in downtown Portland Oregon. We utilize both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, sports injuries, degenerative diseases, infections, tumors and congenital disorders.
Our mission is to return our patients back to pain-free mobility and full strength as quickly and painlessly as possible using both surgical and non-surgical orthopedic procedures.
Our expert physicians provide leading-edge, comprehensive care in the diagnosis and treatment of orthopedic conditions, including total joint replacement and sports medicine. We apply the latest state-of-the-art techniques in order to return our patients to their active lifestyle.
If you’re looking for compassionate, expert orthopedic surgeons in Portland Oregon, contact OSM today.
Phone:
503-224-8399
Address
1515 NW 18th Ave, 3rd Floor
Portland, OR 97209
Hours
Monday–Friday
8:00am – 4:30pm








 Because of the unique properties of their bones, there are some defined fracture subtypes that present only in children. For example:
Because of the unique properties of their bones, there are some defined fracture subtypes that present only in children. For example: